
Enhancing the management of acute and gangrenous cholecystitis: a systematic review supported by the TriNetX database
Introduction
Acute cholecystitis (AC) is a common cause of emergency hospital admission that should be managed according to international guidelines (1,2). It can be classified into 3 grades of severity (mild, moderate, and severe): these grades affect the length of hospital stay, conversion to open surgery, medical costs, and prognosis. Gangrenous cholecystitis (GC) is a severe form of AC (1) and is characterized by gallbladder inflammation with eventual progressive necrosis of the wall and subsequent infection, initially localized and later becoming systemic.
In some cases, the bacterial strains involved in the infection lead to the formation of gas within the gallbladder or in the context of its wall known as emphysematous cholecystitis (EC). Historically, Kirchmayr, in 1925 (3) was the first to draw attention to this condition, while it was Hegner, in 1931, who first recognized the typical roentgen findings of this disease (4).
Except for a few sporadic cases reported in the early 20th century, the first case series of 20 EC (with necrosis and infection caused by gas-producing bacteria) was described in 1999 by Garcia-Sancho Tellez et al. (5).
EC is one of the most life-threatening forms of AC, with low morbidity, averaging from 1% to 3%, while the mortality rate is as high as 25% (6). The presenting symptoms of GC/EC are sometimes very vague and initially indistinguishable from those of uncomplicated AC (7), with fever and right hypochondrial pain as the most common (5).
Rationale and knowledge gap
The lack of cohort and retrospective studies with adequately representative samples still constitutes a limitation in assessing the pathology, both regarding clinical presentation and in establishing the correct therapeutic timing and treatment modalities today. Due to the rarity of their presentation, no literature reviews on EC and GC have been conducted, as most reported cases were sporadic or involved small retrospective case series.
To better understand the existing differences between cases of GC and the more common AC, the international TriNetX database was used for the first time to compare clinical and outcome data of operated and non-operated cases of AC with those obtained from the available literature on cases of GC.
Objective
The aim of this study is to perform a systematic review with the intent of identifying consistent aspects of symptom presentation, diagnosis, and treatment, including recent advances in the field of surgery. This is implemented for the first time with the characteristics of AC collected using a broad-spectrum international database. The review was not registered and no review protocol was prepared. This manuscript is written in accordance with the PRISMA reporting checklist (available at https://tgh.amegroups.com/article/view/10.21037/tgh-24-27/rc).
Methods
Data retrieval
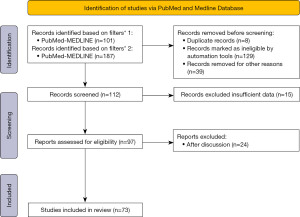
A total of 981 articles in the English language were initially identified in the PubMed-MEDLINE databases using filters for “(emphysematous) AND (cholecystitis)” and “(gangrenous) AND (cholecystectomy)”. After filtering, 288 articles were identified as free full-text articles, focusing on adult patients. Subsequently, following a double-blind review with the input of a third author in case of conflicts, 97 articles were selected for further evaluation. Further scrutiny led to the exclusion of 13 articles due to insufficient data and 11 articles for their limited relevance to the study objectives. Ultimately, 73 articles were deemed suitable for inclusion in the study (Figure 1).
To better understand the results derived from the literature review and the data extracted from the TriNetX database, it was decided to use the classic case report format, organizing the chapters as follows: clinical presentation, diagnosis, and treatment.
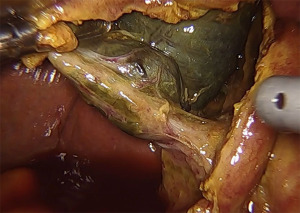
Written informed consent was obtained from the patient for the publication of the specific image in this study. A copy of the written consent is available for review by the editorial office of this journal.
Utilization of TriNetX database
Global-based data from the TriNetX network, a multinational collaborative clinical research platform, were employed for the study. This platform captures real-time medical records encompassing demographics, diagnoses, procedures, medications, laboratory values, and vital statuses. The network consisted of 113 healthcare organizations at the time of analysis, contributing data from approximately 136.4 million patients. Access to the TriNetX network occurred on 11 February 2024, and data extraction and analysis were conducted from the Global Collaborative Network on the TriNetX platform between 11 and 13 February 2024. TriNetX’s built-in analytic functions enabled patient-level analyses while reporting population-level data. The Metro Health System institutional review board deemed the use of data from TriNetX exempt from human subject research approval.
Search and analysis on TriNetX
The database search focused on the electronic medical records of patients aged at least 18 years, of both sexes, diagnosed with AC according to the International Classification of Diseases (ICD)-10 code K81.0. After inclusion in the analyses, the study population underwent evaluation based on demographic (race, sex, and age), anamnestic characteristics (overweight or obesity, hypertension, diabetes mellitus, disorders of lipid metabolism, chronic kidney disease, ischemic heart disease, cerebrovascular diseases, chronic obstructive pulmonary disease, malignancies) and use of medications. Subsequently, the overall population was divided into two groups based on the therapeutic approach for managing AC, distinguishing between exclusively medical or surgical interventions. The study’s ultimate aim was to compare the 5-year all-cause mortality of patients diagnosed with AC treated with or without surgery.
Statistical analysis
We assessed the baseline characteristics of each group using the chi-square test for categorical variables and the Student’s t-test for continuous variables. To balance the cohorts based on these baseline characteristics, we employed propensity score matching, with a 1:1 matching adjusted for covariates that might confound the predefined cardiovascular outcomes. This ensured our cohorts were comparable in terms of demographic variables (age, sex, and race, categorized as white, black or African American, Asian, or other), cardiovascular risk-related health conditions (overweight or obesity, hypertension, diabetes mellitus, lipid metabolism disorders, chronic kidney disease, ischemic heart disease, cerebrovascular diseases, chronic obstructive pulmonary disease) as documented in ICD-10-CM codes in electronic medical records, and the use of specific medications (gastric medications and antilipemic agents).
We performed Kaplan-Meier analyses to estimate the probability of outcomes, specifically all-cause mortality and acute peritonitis, from the index date up to 5 years. Cohort comparisons were conducted using the log-rank test due to consistent differences in the risk of events between the groups. We calculated risk ratios (RRs) and odds ratios (ORs) for each outcome, along with their 95% confidence intervals (CI), and tested for proportionality using the scaled Schoenfeld residuals with R’s Survival package v3.2.3.
All statistical analyses were conducted within TriNetX software, with statistical significance set at a two-sided P<0.05.
Results
Our literature review involved clinical studies with a total of 2,029 patients. We found 9 retrospective studies, with the largest study encompassing 351 patients, and 3 prospective studies, the largest of which involved 474 patients. Additionally, we analyzed 70 patients from 62 case reports and case series included in a database and utilized for descriptive analyses (Table 1).
Table 1
| Authors | Year | Article details | Sample size | Type of study | |
|---|---|---|---|---|---|
| Journal of publication | PMID | ||||
| Williams et al. (8) | 1976 | Can Med Assoc J | 1000456 | 19 | Retrospective |
| Stefanidis et al. (9) | 2005 | JSLS | 15984704 | 238 | Retrospective |
| Nikfarjam et al. (10) | 2011 | HPB (Oxford) | 21762298 | 106 | Retrospective |
| Wu et al. (11) | 2014 | HPB (Oxford) | 24635779 | 351 | Retrospective |
| Mok et al. (12) | 2014 | Int J Surg | 24856179 | 16 | Prospective |
| Önder et al. (13) | 2015 | Int Surg | 25692427 | 107 | Retrospective |
| Gomes et al. (14) | 2019 | Ann Hepatobiliary Pancreat Surg | 30863805 | 95 | Retrospective |
| Shirah et al. (15) | 2019 | Ann Hepatobiliary Pancreat Surg | 31501810 | 117 | Retrospective |
| Alghamdi et al. (16) | 2019 | Mater Sociomed | 32082095 | 57 | Retrospective |
| Díez Ares et al. (17) | 2021 | Rev Esp Enferm Dig | 33054305 | 127 | Prospective |
| Rahimli et al. (18) | 2022 | BMC Surg | 35538571 | 252 | Retrospective |
| De Simone et al. (19) | 2022 | World J Emerg Surg | 36527038 | 474 | Prospective |
GC, gangrenous cholecystitis; EC, emphysematous cholecystitis.
Analyzing the data from the TriNetX database, we identified a total sample of 245,668 patients who were hospitalized for AC, 56% of whom were female with a significantly higher percentage of females in both groups of operated and non-operated subjects (P<0.001). Approximately one-third of the patients (n=96,455) did not undergo surgery, while the age of non-operated patients was higher than that of operated ones (66±19, 58±19; P<0.001).
Significant differences were found also in terms of race, with the white one generally more represented in both groups, much more than any others.
Among the most frequent comorbidities observed in the study population, hypertension was the highest (37%), followed by disorders of lipid metabolism (27%), overweight (20%), diabetes mellitus (18%), ischemic heart disease (15%), chronic kidney disease (9%), cerebrovascular diseases (8%), and chronic obstructive pulmonary disease (16%).
While overweight or obesity was more frequent in the surgery group (24% vs. 14%, P<0.001), hypertension, diabetes mellitus, ischemic heart disease, chronic kidney disease and cerebrovascular diseases were more frequent in the non-operated patients (37% vs. 36%; 20% vs. 17%; 19% vs. 13%; 12% vs. 8%; 11% vs. 6%, respectively; all with P<0.001).
Significant differences were observed in the percentages of patients receiving gastric medications [not exclusively but prevalently proton pump inhibitors (PPIs)] and antilipemic agents (also in this case not exclusively but prevalently statins): the data concerning gastric medications is particularly eloquent, since 43% of operated patients were treated with such drugs versus 33% of non-operated subjects (P<0.001) (Table 2).
Table 2
| Variables | Overall population (n=245,668) | No surgery (n=96,455) | Surgery (n=149,213) | P |
|---|---|---|---|---|
| Age, years, mean ± standard deviation | 61±19 | 66±19 | 58±19 | <0.001 |
| Sex, n (%) | ||||
| Male | 107,038 (44) | 44,369 (46) | 62,669 (42) | <0.001 |
| Female | 138,630 (56) | 52,086 (54) | 86,544 (58) | |
| Race, n (%) | ||||
| White | 142,578 (58) | 53,050 (55) | 89,528 (60) | <0.001 |
| Black or African American | 23,075 (9) | 9,646 (10) | 13,429 (9) | <0.001 |
| Asian | 9,827 (4) | 3,858 (4) | 5,969 (4) | 0.76 |
| Others | 70,188 (29) | 29,901 (31) | 40,287 (27) | <0.001 |
| Comorbidities, n (%) | ||||
| Overweight or obesity | 49,395 (20) | 13,541 (14) | 35,854 (24) | <0.001 |
| Hypertension | 89,813 (37) | 35,890 (37) | 53,923 (36) | <0.001 |
| Diabetes mellitus | 44,207 (18) | 18,914 (20) | 25,293 (17) | <0.001 |
| Disorders of lipid metabolism | 67,324 (27) | 26,312 (27) | 41,012 (27) | 0.88 |
| Chronic kidney disease | 23,083 (9) | 11,781 (12) | 11,302 (8) | <0.001 |
| Ischemic heart disease | 37,487 (15) | 17,847 (19) | 19,640 (13) | <0.001 |
| Cerebrovascular diseases | 19,921 (8) | 10,383 (11) | 9,538 (6) | <0.001 |
| Chronic obstructive pulmonary disease | 38,504 (16) | 15,250 (16) | 23,254 (16) | 0.13 |
| Medications, n (%) | ||||
| Gastric medications | 96,255 (39) | 31,778 (33) | 64,477 (43) | <0.001 |
| Antilipemic agents | 55,464 (23) | 22,541 (23) | 32,923 (22) | <0.001 |
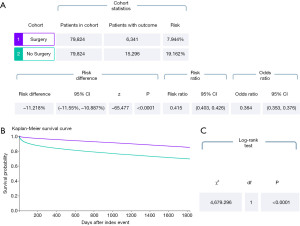
As for Kaplan-Meier analyses, we focused our attention on the differences between the two major groups considered (operated vs. non-operated subjects with AC), finding how the patients who underwent surgery for AC presented generally lower mortality rates in the whole period of follow-up extended to 5 years (RR 0.415, 95% CI: 0.403–0.426; OR 0.364, 95% CI: 0.353–0.376; P<0.001) and this was particularly evident in the first 200 days of observation since index event (Figure 2).
Discussion
Attention to the clinical-pathological condition of GC has increased over the years, as evidenced by the growing number of retrospective and prospective studies; 9 out of the 12 found have been conducted in the last 10 years. This is likely due, in part, to an increase in cases overall involving older and more vulnerable individuals, following the increase in life expectancy. Below, we report the main characteristics of the articles included in the study, organizing the information by topics.
Clinical presentation
A plausible explanation for the development of GC seems to involve epithelial damage, which leads to an elevation in gallbladder wall tension due to vascular insufficiency resulting from persistent obstruction of the cystic duct. This sequence of events contributes to the swift progression of GC. Moreover, phospholipases released from damaged epithelial cell membranes trigger a vigorous inflammatory reaction, ultimately resulting in increased rates of necrosis and perforation (13). EC is considered one of the most life-threatening forms of AC, with a relatively low morbidity rate ranging from 1% to 3%; however, the mortality rate associated with EC is notably high, reaching up to 25% (6).
Distinguishing EC from gallstone-related AC or acute obstructive suppurative cholangitis (AOSC) solely based on symptoms and signs poses a challenge. EC typically manifests in male patients aged 50–70 years, frequently in individuals with comorbidities such as diabetes mellitus, immunosuppression, and peripheral vascular disease (7,12); fever, nausea, and vomiting constitute the primary clinical symptoms.
The condition often arises from thrombosis or occlusion of the cystic artery, leading to ischemic necrosis of the gallbladder wall, with subsequent gallbladder necrosis, and secondary infection by gas-forming organisms. EC can be categorized into three variants: gas in the gallbladder lumen, gallbladder wall, and pericholecystic tissues.
However, the initial EC symptoms can sometimes be vague and indistinguishable from those of uncomplicated AC. In diabetic individuals, for example, an environment conducive to submucosal thrombosis of the biliary tract may be created, predisposing patients to fulminant infections: undiagnosed diabetic neuropathy might contribute to a delayed diagnosis by masking symptoms of an acute abdomen. In diabetic subjects, hyperglycemia and ischemic conditions may impede phagocyte mobility in infected areas, thereby reducing antimicrobial activity and increasing the likelihood of EC (7).
In contrast to more recent clinical cases, a 1976 article documented 496 patients diagnosed with AC, of which 19 had gallbladder perforation. The average age in this cohort was 69 years, and the female-to-male ratio was 3:2 (8).
However, several retrospective studies have identified male sex, older age groups, and the white blood cell (WBC) count of more than 14,000 as factors associated with GC (12).
In a retrospective study conducted only on male patients, significant risk factors for gallbladder complications were diabetes mellitus, gallbladder thickness greater than 4 mm, elevated gamma-glutamyl transferase (GGT), and leukocytosis. Lastly, Murphy’s sign was identified as a protective factor against gallbladder necrosis (14).
A review of 5,812 patients undergoing cholecystectomy revealed a low preoperative ability to diagnose gallbladder complications, encompassing only 9% of cases. Specific factors, such as age over 45 years, heart rate over 90 bpm, leukocyte count over 13,000/mm3, gallbladder wall thickness over 4 mm, the presence of pericolic fluid in ultrasound (US), and an American Society of Anesthesiology (ASA) score over 2, showed a 63% probability of gallbladder complications when all these factors were present (10,12,15).
Cholecystitis as a complication of endoscopic retrograde cholangiopancreatography (ERCP) is rare, with only three reported cases of postprocedural EC. In one case, recurrent post-operative episodes of biliary obstruction, cholangitis, and sepsis led to secondary biliary cirrhosis requiring liver transplantation (20).
Patient age was identified as a significant factor in developing gallbladder complications, while male sex was a factor with no observed correlation. WBC count and total bilirubin levels were within normal ranges, and symptoms such as vomiting, fever, and nausea were less pronounced compared to other studies. Computed tomography (CT) did not provide significant support and did not play a crucial role in detecting gallbladder complications (16).
Diagnosis
Due to the differing prognosis of AC based on the degree of inflammation, early detection and prompt operation for severe cholecystitis are crucial for successful treatment. However, CT has limited discriminative value in distinguishing between uncomplicated and severe cholecystitis (21).
US is considered the optimal initial imaging modality for detection, although its effectiveness in visualizing EC varies depending on the amount of air in the gallbladder (22).
Magnetic resonance cholangiopancreatography (MRCP) is essential for the non-invasive investigation of pancreatic-biliary disorders, having significantly advanced over the years due to improvements in spatial and temporal resolution. Despite these advancements, MRCP is not routinely performed prior to cholecystectomy. Instead, it is reserved for specific clinical scenarios, such as suspected choledocholithiasis and situations where delaying the surgical procedure is feasible (23).
Recent Tokyo guidelines have introduced a complex scoring system based on clinical, biochemical, and radiological criteria for severity grading of AC. However, these scoring systems, while reliably predicting gallbladder complications, lack simplicity and practical application. Therefore, there is still a need to identify simple risk scores that can aid in early surgical evaluation and urgent intervention (24).
Yacoub et al. developed a score, identifying five independent variables associated with GC: Male sex (2 points), WBC count >13,000 (1.5 points), heart rate >90 (1 point), gallbladder wall thickness >4.5 mm, and age >45 years. A clinical score >4.5 had a positive predictive value nearing 90%, allowing accurate classification into low, intermediate, or high probabilities of GC (25).
The Yacoub score was externally validated by Wu et al., with 0 points indicating a 2% probability of GC, and 5 points indicating a 63% probability (11).
Similarly, a prospective cohort study involving 117 cases of GC concluded that gallbladder sonographic wall thickness of 5.1–6 mm or more than 6 mm, male sex, diabetes mellitus, leukocytosis >15,000 cells/mL, and age ≥40 years were factors predisposing to gangrene-complicated acute calculous cholecystitis. Other risk factors such as high alanine aminotransferase (ALT), elevated aspartate aminotransferase (AST), and high alkaline phosphatase (ALP) could assist in the decision for early operation (15).
The association of GC with high C-reactive protein (CRP) levels has been consistently observed as well.
Several retrospective studies have identified male sex, older age groups, and a WBC count of more than 14,000 as associated with the development of GC (12). In another study, Nikfarjam et al. found significantly higher CRP levels in patients with GC compared to those with non-GC (10).
As for example, Gill et al. radiographically divided EC into three stages based on the distribution of air within the gallbladder and/or the biliary system: stage 1—air in the gallbladder lumen, stage 2—air in the gallbladder wall, and stage 3—air in the pericholecystic tissue (26).
Another rare condition that could affect the gallbladders is torsion which has been reported in approximately 400 cases since it was first described by Wendel in 1898 (27): it occurs three times more frequently in females than in males, and preoperative diagnosis is achieved in only 10% of cases. Torsion of the gallbladder neck typically results in vascular compromise and mural necrosis, with symptoms possibly being intermittent due to the torsion-detorsion phenomenon: a CT scan can reveal the typical “whirl sign” (28).
In the course of 2020, the COVID-19 pandemic led surgeons to postpone surgeries due to the massive healthcare burden that hospitals had to face during the initial waves. In such a situation, the necessity to defer surgeries, even urgent ones, arose. This behavior represented an anomaly of unprecedented scale, and the effects of this conduct were captured by a retrospective study exploited during the COVID-19 pandemic.
A retrospective study conducted during the COVID-19 pandemic on 252 patients showed that the elderly patients were diagnosed more frequently with GC compared with other patients (18); moreover, the authors stated that laparoscopic biliary surgery was generally safe, also in in the COVID-19 era without negative impact on perioperative results.
The only available prospective study conducted on 474 patients with GC-EC during the COVID-19 era focused on the role of SARS-CoV-2 in the pathology of acute GC: authors analyzed the role of COVID-19 in patients with AC, specifically by measuring the incidence of GC between the COVID-positive and COVID-negative patient groups. The rationale behind this research was to assess, for the first time, the impact of COVID-19 and its inflammatory cascade on the course of AC. It was hypothesized that the pro-thrombotic nature of the virus could exacerbate cholecystitis due to potential microangiopathic damage: the prospective cohort study (ChoCO-W study, NCT04542312), concluded that the incidence of GC doubled in the COVID-19 group, and emphasized that a CT scan is the first choice for differentially diagnosing possibilities, including AOSC, perforation, and acute pancreatitis (19).
Treatment
Non-surgical treatment experiences for GC have documented a poor therapeutic response. De Jode’s initial article reported conservative treatment with penicillin and tetracycline, with the patient readmitted one month later for traditional cholecystectomy, revealing a residual abscess in a gangrenous gallbladder (29).
Mok and colleagues in their study exploited in 2014 revealed how surgeons were able to diagnose GC preoperatively in only 9% of cases. Patients with GC experienced more complications, including bile duct injury, increased estimated blood loss (EBL), and a higher frequency of open cholecystectomies (12). Contini et al. highlighted that delayed admission was a crucial criterion in the development of GC (30), while Eldar et al. reported worsening laparoscopic alterations in cases of hospital admissions later than 48 hours (31). Several clinical studies have demonstrated that early cholecystectomy plays a crucial role in preventing complications associated with GC. Conversely, delay in operative intervention poses a significant concern (32,33).
The “golden hours of operation” (72–96 hours) since the onset of symptoms have in fact lowered complication rates, reduced conversion rates, shortened hospital stays, and prevented complications (15). In a retrospective study comparing open and laparoscopic cholecystectomy (LC) from 1982 to 1992 and from 1992 to 2002, Stefanidis et al. found that the laparoscopic group had a lower rate of intensive care unit (ICU) admissions (13% vs. 5%), a shorter overall length of hospital stays (10 vs. 5.7 days), and a lower rate of intra-abdominal abscesses (8% vs. 0.7%) (9) (Figure 3).
Recently, fluorescent cholangiography was evaluated as an imaging diagnostic tool and was found comparable to MRCP for detailed intra-operative visualization of the cystic duct-common hepatic duct anatomy during elective laparoscopic cholecystectomies (23).
It is well known that inflammation can alternate anatomical planes during urgent cholecystectomy and may lead to a high risk of biliary or vascular lesions, especially in case of GC.
Near-infrared fluorescent cholangiography (NIRF-C) represents a novel intra-operative imaging technique that allows a real-time enhanced visualization of the extrahepatic biliary tree by fluorescence during surgery (23).
In emergency cholecystectomies, NIRF-C is a safe and effective tool for preventing bile duct injury during LC. However, the current data necessitate further analysis through randomized controlled studies involving larger patient populations with AC undergoing LC with intra-operative fluorescent cholangiography (34).
Recently, percutaneous transhepatic gallbladder drainage (PTGBD) has seen increased use for emergency cholecystitis (EC). However, conservative treatments, including PTGBD, are not considered appropriate for EC due to the high risk of gallbladder necrosis and perforation (35).
Outcome
The most prevalent complications observed in cholecystectomy for GC were chest infections, cardiac complications, and bile leaks. However, individuals in the GC group were more prone to requiring postoperative ICU admission compared to those with uncomplicated AC (15% vs. 7%).
Factors influencing morbidity included age, diabetes, and the identification of muscle rigidity during examination as the sole independent contributors (10,13).
Risk factors associated with postoperative mortality encompassed a longer delay in hospital admission, low WBC count, the presence of diabetes mellitus, elevated blood levels AST, ALT, ALP and total bilirubin, pericholecystic fluid detected in abdominal ultrasonography, and conversion from laparoscopic surgery to open surgery (13).
Garcia-Sancho Tellez et al. reported an approaching 25% mortality rate with morbidity rates reaching 50% (5).
The male-to-female ratio stood at 7:3, and over 40% of EC patients suffered from diabetes mellitus. EC is typically presented in individuals over the age of 50 being characterized by cholecystitis without stones, distinguishing it from common AC (35).
Patients with GC exhibited a higher incidence of complications, including bile duct injury, increased EBL, and a greater frequency of open cholecystectomies (11).
Analyses of TriNetX database
Regarding the TriNetX research, the age of non-operated AC patients was higher than that of operated ones (66±19, 58±19; P<0.001), confirming the trend also observed in the literature review. Moreover, patients with pre-existing co-morbidities at the time of admission were predominantly treated conservatively. This is probably due to a more conservative approach towards frail patients, often elderly, due to the high perioperative risk present in these cases, even if it is not possible to prove it since the analyses were conducted on an administrative database.
In a recent retrospective study conducted from our research group during the lockdown for the first wave of the COVID-19 pandemic, it emerged that the postponement of urgent surgical procedures, including cholecystectomies, did not result in a short-term rebound effect with hospital readmissions for recurrent AC (36).
However, Figure 2, derived from TriNetX’s analyses, highlights how the “surgical intervention” factor is crucial to improve the overall survival of patients diagnosed with AC already in the first 200 days from admission, and then aligns with the non-operated group up to 5 years from the event (P<0.001).
Moreover, about one-third of the sample patients present a diagnosis of obesity or overweight: both factors appear to predispose them to surgical intervention, likely due to the high intake of highly energetic foods rich in lipids and carbohydrates, typical of the dietary habits of obese/overweight patients (37).
Indeed, an obese or overweight patient with gallstones usually persists in maintaining an improper dietary regimen, resulting in recurrent biliary colic. Therefore, surgical intervention is hardly postponable as it cannot adequately and promptly correct the predisposing causes of cholecystitis.
The subjects who did not undergo surgery for AC presented generally a higher load of comorbidities and this regarded hypertension (39% vs. 37%), diabetes mellitus (20% vs. 18%), chronic kidney diseases (13% vs. 8%) and cerebrovascular diseases (11% vs. 7%): in this case it is conceivable that the choice of conservative treatment had been made due to their high perioperative risk and, in this sense, these data do not deserve further explanations.
As for medication use, the role of PPIs was observed to be significant in operated patients for cholecystitis, increasing the risk of undergoing surgery. We searched for similar previous experiences, finding only 2 publications (38,39). These evidenced how, besides beneficial effects, PPIs (one of the most administered drugs worldwide) could also present several side effects such as increased risk of intra-abdominal infections, pseudomembranous colitis, liver abscess and microbiome gut affections.
Consequently, PPIs may theoretically increase the risk of developing AC by promoting the growth of enteric organisms and the risk of secondary infection. In a case-control study involving approximately 3,000 patients, the authors observed a higher proportion of PPI users in the cholecystitis group compared to the control group (36% vs. 29.0%, P<0.001). After adjusting for comorbidities, PPI users still had a 1.23-fold increased risk of cholecystitis compared to PPI non-users (OR 1.23, 95% CI: 1.13–1.34).
It is generally hypothesized that PPIs decrease gastric acid secretion, increase the stomach’s pH, reduce bactericidal activity, and allow pathogens to pass through the stomach to the duodenum. This process potentially increases the risk of retrograding migration to the biliary system, thereby elevating the incidence of biliary tract infections, including AC.
One study involving 211 PPI users analyzed their stool samples, revealing a significant increase in bacteria, including Enterococcus, Streptococcus, Staphylococcus, and Escherichia coli, some of which are common pathogens in AC (38).
To our knowledge, our study is the first to confirm, with external validation on a wide cohort, the same hypothesis.
Antilipemic agents also appeared to have a protective effect on the development of AC, being more prevalent in the group of non-operated patients. A possible correlation between hypercholesterolemia and AC could be justified by the high incidence of both conditions in overweight patients and the role of antilipemic agents in controlling hypercholesterolemia, which likely limits the formation of cholesterol stones in the gallbladder (40,41).
Limitations and bias
Our study has several limitations and many of them are related to the lack of large evidence dedicated to the topics. As for the patients with AC, we decided to query the TriNetX database, which is composed of administrative data: if on one hand it is able to exploit analyses deriving them from a large amount of data, the retrospective nature of the analyses themselves represents probably the most important limitation.
Furthermore, the administrative nature of the data represents a selection bias, that cannot be overcome.
As for the cohort of subjects enrolled in the analysis, it should be underlined that they were predominantly of Caucasian race, which may have further biased the sample characteristics.
Additionally, the TriNetX database does not allow for multivariate investigations and, therefore, the results of this study refer exclusively to univariate comparisons of the selected variables; in this case, the populations chosen (operated vs. non-operated for AC) were matched to reduce the imbalance between groups towards the selected outcomes.
Concerning the literature review, articles often did not have the same structure (for example, most case reports lacked some fundamental data), and this did not always make all the information on patient characteristics available.
Based on what has been said, further research is necessary to confirm or to refuse these preliminary findings and our study can serve as the basis for increasing knowledge in the field of acute, gangrenous and EC.
Conclusions
In subjects with AC, non-surgical treatments seem generally less effective in reducing 5-year all-cause mortality and it is particularly evident in the first 200 days post-hospitalization.
Timely surgical intervention within the “golden hours of operation” (72–96 hours) may reduce complications, such as conversion rates, infections, and the length of hospital stays. Laparoscopic surgery, in this sense, has been found to decrease the rate of ICU, the overall length of hospital stays, and the occurrence of intra-abdominal abscesses.
PPIs appear to increase the risk of undergoing surgical intervention for AC and its role deserves to be further explored in larger studies.
Acknowledgments
The authors thank Dr. R. Lordi for the data analysis.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tgh.amegroups.com/article/view/10.21037/tgh-24-27/rc
Peer Review File: Available at https://tgh.amegroups.com/article/view/10.21037/tgh-24-27/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tgh.amegroups.com/article/view/10.21037/tgh-24-27/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for the publication of the specific image. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yokoe M, Hata J, Takada T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2018;25:41-54. [Crossref] [PubMed]
- Pisano M, Allievi N, Gurusamy K, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg 2020;15:61. [Crossref] [PubMed]
- Kirchmayr L. Ueber einem Fall von Gasbrand der Gallenblase. Zentralbl f Chir 1925;52:1522-7.
- Hegner CF. Gaseous pericholecystitis with cholecystitis and cholelithiasis. Arch Surg 1931;22:993-1000. [Crossref]
- Garcia-Sancho Tellez L, Rodriguez-Montes JA, Fernandez de Lis S, et al. Acute emphysematous cholecystitis. Report of twenty cases. Hepatogastroenterology 1999;46:2144-8. [PubMed]
- Chen MY, Lu C, Wang YF, et al. Emphysematous cholecystitis in a young male without predisposing factors: A case report. Medicine (Baltimore) 2016;95:e5367. [Crossref] [PubMed]
- Liao CY, Tsai CC, Kuo WH, et al. Emphysematous cholecystitis presenting as gas-forming liver abscess and pneumoperitoneum in a dialysis patient: a case report and review of the literature. BMC Nephrol 2016;17:23. [Crossref] [PubMed]
- Williams NF, Scobie TK. Perforation of the gallbladder: analysis of 19 cases. Can Med Assoc J 1976;115:1223-5. [PubMed]
- Stefanidis D, Bingener J, Richards M, et al. Gangrenous cholecystitis in the decade before and after the introduction of laparoscopic cholecystectomy. JSLS 2005;9:169-73. [PubMed]
- Nikfarjam M, Niumsawatt V, Sethu A, et al. Outcomes of contemporary management of gangrenous and non-gangrenous acute cholecystitis. HPB (Oxford) 2011;13:551-8. [Crossref] [PubMed]
- Wu B, Buddensick TJ, Ferdosi H, et al. Predicting gangrenous cholecystitis. HPB (Oxford) 2014;16:801-6. [Crossref] [PubMed]
- Mok KW, Reddy R, Wood F, et al. Is C-reactive protein a useful adjunct in selecting patients for emergency cholecystectomy by predicting severe/gangrenous cholecystitis? Int J Surg 2014;12:649-53. [Crossref] [PubMed]
- Önder A, Kapan M, Ülger BV, et al. Gangrenous cholecystitis: mortality and risk factors. Int Surg 2015;100:254-60. [Crossref] [PubMed]
- Gomes CA, Soares C, Di Saverio S, et al. Gangrenous cholecystitis in male patients: A study of prevalence and predictive risk factors. Ann Hepatobiliary Pancreat Surg 2019;23:34-40. [Crossref] [PubMed]
- Shirah BH, Shirah HA, Saleem MA, et al. Predictive factors for gangrene complication in acute calculous cholecystitis. Ann Hepatobiliary Pancreat Surg 2019;23:228-33. [Crossref] [PubMed]
- Alghamdi KA, Rizk HA, Jamal WH, et al. Risk Factors of Gangrenous Cholecystitis in General Surgery Patient Admitted for Cholecystectomy in King Abdul-Aziz University Hospital (KAUH), Saudi Arabia. Mater Sociomed 2019;31:286-9. [Crossref] [PubMed]
- Díez Ares JÁ, Martínez García R, Estellés Vidagany N, et al. Can inflammatory biomarkers help in the diagnosis and prognosis of gangrenous acute cholecystitis? A prospective study. Rev Esp Enferm Dig 2021;113:41-4. [PubMed]
- Rahimli M, Wex C, Wiesmueller F, et al. Laparoscopic cholecystectomy during the COVID-19 pandemic in a tertiary care hospital in Germany: higher rates of acute and gangrenous cholecystitis in elderly patients. BMC Surg 2022;22:168. [Crossref] [PubMed]
- De Simone B, Abu-Zidan FM, Chouillard E, et al. The ChoCO-W prospective observational global study: Does COVID-19 increase gangrenous cholecystitis? World J Emerg Surg 2022;17:61. [Crossref] [PubMed]
- Bari K, Aslanian HR, Pollak J, et al. Emphysematous Cholecystitis Resulting in Secondary Biliary Cirrhosis: A Rare Complication of Endoscopic Retrograde Cholangiopancreatography. ACG Case Rep J 2013;1:51-4. [Crossref] [PubMed]
- Kim KH, Kim SJ, Lee SC, et al. Risk assessment scales and predictors for simple versus severe cholecystitis in performing laparoscopic cholecystectomy. Asian J Surg 2017;40:367-74. [Crossref] [PubMed]
- Kunadia A, Leong MB, Komanduri K, et al. Emphysematous Cholecystitis Secondary to Fusobacterium nucleatum. Cureus 2021;13:e15660. [PubMed]
- Pesce A, La Greca G, Esposto Ultimo L, et al. Effectiveness of near-infrared fluorescent cholangiography in the identification of cystic duct-common hepatic duct anatomy in comparison to magnetic resonance cholangio-pancreatography: a preliminary study. Surg Endosc 2020;34:2715-21. [Crossref] [PubMed]
- Mayumi T, Okamoto K, Takada T, et al. Tokyo Guidelines 2018: management bundles for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 2018;25:96-100. [Crossref] [PubMed]
- Yacoub WN, Petrosyan M, Sehgal I, et al. Prediction of patients with acute cholecystitis requiring emergent cholecystectomy: a simple score. Gastroenterol Res Pract 2010;2010:901739. [Crossref] [PubMed]
- Gill KS, Chapman AH, Weston MJ. The changing face of emphysematous cholecystitis. Br J Radiol 1997;70:986-91. [Crossref] [PubMed]
- Wendel AV. VI. A Case of Floating Gall-Bladder and Kidney complicated by Cholelithiasis, with Perforation of the Gall-Bladder. Ann Surg 1898;27:199-202. [PubMed]
- Rosenblum JK, Dym RJ, Sas N, et al. Gallbladder torsion resulting in gangrenous cholecystitis within a parastomal hernia: findings on unenhanced CT. J Radiol Case Rep 2013;7:21-5. [Crossref] [PubMed]
- De Jode LR. Total Necrosis of Gall-bladder after Emphysematous Cholecystitis: Recovery. Br Med J 1960;2:1855-6. [Crossref] [PubMed]
- Contini S, Corradi D, Busi N, et al. Can gangrenous cholecystitis be prevented?: a plea against a "wait and see" attitude. J Clin Gastroenterol 2004;38:710-6. [Crossref] [PubMed]
- Eldar S, Eitan A, Bickel A, et al. The impact of patient delay and physician delay on the outcome of laparoscopic cholecystectomy for acute cholecystitis. Am J Surg 1999;178:303-7. [Crossref] [PubMed]
- Fagan SP, Awad SS, Rahwan K, et al. Prognostic factors for the development of gangrenous cholecystitis. Am J Surg 2003;186:481-5. [Crossref] [PubMed]
- Shpitz B, Sigal A, Kaufman Z, et al. Acute cholecystitis in diabetic patients. Am Surg 1995;61:964-7. [PubMed]
- Pesce A, Piccolo G, Lecchi F, et al. Fluorescent cholangiography: An up-to-date overview twelve years after the first clinical application. World J Gastroenterol 2021;27:5989-6003. [Crossref] [PubMed]
- Funahashi H, Komori T, Sumita N. Successful treatment of emphysematous cholecystitis by laparoscopic surgery. J Surg Case Rep 2021;2021:rjab080. [Crossref] [PubMed]
- Fabbri N, Pesce A, Uccellatori L, et al. Long term Implications in Surgical re-Assisting (L.I.S.A. study) during the Covid-19 outbreak. A retrospective observational cohort study on a rural population. Ann Ital Chir 2023;94:195-202. [PubMed]
- Jeong SU, Lee SK. Obesity and gallbladder diseases. Korean J Gastroenterol 2012;59:27-34. [Crossref] [PubMed]
- Imhann F, Bonder MJ, Vich Vila A, et al. Proton pump inhibitors affect the gut microbiome. Gut 2016;65:740-8. [Crossref] [PubMed]
- Chuang SC, Lin CC, Peng CY, et al. Proton pump inhibitors increase the risk of cholecystitis: a population-based case-control study. Gut 2019;68:1337-9. [Crossref] [PubMed]
- Yoon JH, Kim YJ, Baik GH, et al. The Impact of Body Mass Index as a Predictive Factor of Steatocholecystitis. Hepatogastroenterology 2014;61:902-7. [PubMed]
- Parra-Landazury NM, Cordova-Gallardo J, Méndez-Sánchez N. Obesity and Gallstones. Visc Med 2021;37:394-402. [Crossref] [PubMed]
Cite this article as: Fabbri N, Greco S, Pesce A, Virgilio F, Bonazza L, Bagnoli L, Feo CV. Enhancing the management of acute and gangrenous cholecystitis: a systematic review supported by the TriNetX database. Transl Gastroenterol Hepatol 2025;10:16.


