Application and effectiveness of an improved endoscopically guided nasojejunal tube placement technique in critically ill patients: a retrospective cohort study
Highlight box
Key findings
• We improved the traditional endoscopically guided technique by incorporating an extra silk thread knot to assist accurate tube placement.
What is known and what is new?
• The conventional endoscopy-guided tube insertion method presents issues of excessive procedural duration.
• The improved endoscopically guided nasojejunal (NJ) tube placement technique is a rapid and safe procedure with excellent patient tolerance, which significantly improves the nutritional status of critically ill patients.
What is the implication, and what should change now?
• The improved endoscopically guided NJ tube placement technique emerges as a viable option for enteral nutrition intervention in critically ill patients.
Introduction
Critically ill patients facing a heightened nutritional risk due to severe trauma and infection require timely intervention with enteral nutrition (EN) (1-3). Beyond providing energy support such as parenteral nutrition, EN also plays a crucial role in preserving the functional integrity of the intestinal barrier, thereby reducing the risk of infections and organ failure, shortening hospital stays, and yielding cost savings in medical care (1,4-8). In cases where gastrointestinal complications disrupt EN administration, posterior pyloric feeding through a nasojejunal (NJ) feeding tube is recommended to facilitate optimal nutrition supplementation.
Several methods exist for the correct placement of the NJ feeding tube, with the endoscopically guided technique considered the gold standard, boasting a success rate of approximately 90–95% (9-11). Compared with the fluoroscopic technique and guide wire technique, the endoscopic technique has its own superiority in safety and convenience in operation, which depends on experienced endoscopists. However, the traditional endoscopic approach still presents challenges concerning the depth and speed of tube insertion, particularly for less experienced practitioners. Addressing the issue of easing NJ tube placement into the jejunum remains crucial for the success of the endoscopically guided technique, which allows novice medical practitioners to acquire this skill more rapidly (12).
Recently, we improved the traditional catheterization method by incorporating a silk knot at the 25 cm mark of the intestinal segment of the NJ tube. This modification enables endoscopic doctors to use biopsy forceps to grasp the silk knot and assist the NJ tube in passing through the pylorus and duodenum, which renders NJ tube placement much faster and more convenient. Here, we introduce the modified endoscopic method and report our evaluation of the safety and usefulness of this new technique in 88 critically ill patients. We present this article in accordance with the STROBE reporting checklist (available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-87/rc).
Methods
Patients
We retrospectively analyzed the intubation time and nutritional status after intubation in critically ill patients who received improved endoscopic guide NJ catheterization. Critically ill patients receiving NJ feeding therapy at Sun Yat-sen Memorial Hospital from January 1, 2020, to March 31, 2023, were collated for analysis. Patients were enrolled if they met all the following criteria: (I) age ≥18 years old; (II) critically ill patients receiving improved endoscopic guide NJ catheterization; (III) EN therapy lasting at least 7 days; (IV) follow-up ≥14 days. Finally, 88 patients totally who received ventilator therapy in the intensive care unit (ICU) ward due to severe pancreatitis, pneumonia, cerebral hemorrhage, craniocerebral trauma, major operations, etc., were enrolled in this study. Experienced endoscopists performed modified endoscopic guide NJ catheterization on these patients for follow-up EN support treatment.
Several laboratory parameters and complication data of patients before and 7 days post EJ catheterization were collected. The tolerance score for EN was calculated via the gastrointestinal adverse reactions post-EJ feeding therapy to assess the tolerance and adverse reactions associated with EN.
This study was approved by the Sun Yat-sen Memorial Hospital Ethics Committee (No. LX-HG-2023096) and conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent from participants was exempted due to the retrospective nature of the study.
Procedure of improved endoscopic guide NJ catheterization
Three-cavity NJ catheterization (16 Fr) was used for EN therapy. All NJ tube placements were finished by an experienced endoscopic doctor and an experienced endoscopic nurse. The preparation before the operation included fasting for 4–6 h, water deprivation for 2 h, and posterior oropharynx anesthesia with 4% xylocaine. The entire time of the catheterization procedure was calculated from the NJ tube into the nasal cavity.
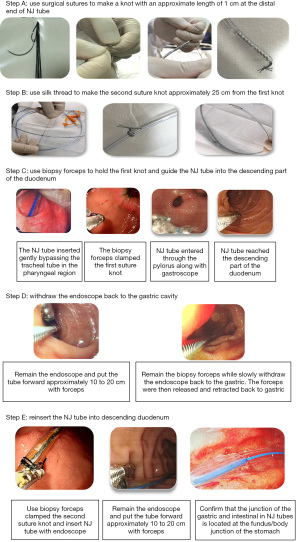
Before intubation, preparatory steps were undertaken on the NJ tube to facilitate its subsequent insertion. Two surgical knots were created at the tip of the NJ tube using absorbable suture material. The first knot was situated at the tube’s end, spanning a length of 1 cm, while the second knot was placed 25 cm away from the first knot (Figure 1, Steps A and B). It is important to note that the surgical knot at the tail end required penetration by a suture needle, and the knot was continuously tightened until it reached a length of approximately 1 cm. This method effectively prevented slippage or loosening of the silk knot during the placement of the tube.
With the NJ tube lubricated, it was inserted into the gastric region. Under endoscopic guidance, biopsy forceps were employed to grasp the first silk knot and maneuver the NJ tube through the pylorus into the descending duodenum (Figure 1, Step C). Subsequently, the gastroscope remained in the descending duodenum, while the biopsy forceps, with the clamped silk knot, were advanced by 10 to 20 cm. While maintaining the position and tension of the biopsy forceps, the gastroscope was slowly withdrawn back into the gastric cavity, and then the biopsy forceps were gradually retracted to the gastric region (Figure 1, Step D). Next, the second knot was grasped by biopsy forceps, and the tube was directed into the pylorus and descending duodenum with the assistance of the endoscope. After confirming that the junction of the NJ tube in the gastric and intestinal regions was positioned at the junction of the fundus/body of the stomach and ensuring that the NJ tube was not twisted or entangled, the guide wire was removed. Subsequently, the endoscope was gently withdrawn from the mouth (Figure 1, Step E). During endoscope withdrawal, the doctor gently oscillated the endoscope to reduce friction with the NJ tube, while the nurse maintained slight pressure on the NJ tube in the patient’s nasal cavity to prevent tube dislodgment.
After ensuring the patency of the lumen, the NJ tube was fixed, and X-ray was used to confirm that the end of the NJ tube was located at the L3 level, which was considered to be located in the projected area of the upper jejunum.
Statistical analysis
Continuous variables are shown herein as the mean ± standard deviation. A paired t-test was used to compare the mean values of paired samples. SPSS 22.0 (International Business Machines Corporation, USA) was applied to perform the statistical analysis, and GraphPad Prism 9.0 (GraphPad Software, LLC, USA) was used for image analysis. All statistical tests were two-sided with statistical significance accepted at P<0.05.
Results
Clinical characteristics
In this study, a total of 88 critically ill patients from the ICU ward were enrolled. The detailed characteristics of these patients are listed in Table 1. Following the improved NJ catheter placement, these 88 critically ill patients, with an average age of 59.6±15.5 years and a male ratio of 86.4%, received a mean of 21 [min–max: 7–25] days of EN therapy. Most of them had poor nutrition risks and needed EN therapy due to major operations, cerebrovascular disease, severe pancreatitis, etc. The average depth of catheterization was 108.8±12.5 cm, and the average time of catheterization was approximately 5.9±2.2 min, which was found to be better than the traditional endoscopically guided approach (nearly 14 min) (9). During the mean 21 [min–max: 7–25] days of EN support, most patients could tolerate EN therapy well, with an average tolerance score of 0.79 for EN. Except for 3 patients who died of severe primary disease, the remaining patients completed the EN therapy until they recovered to resume a regular diet.
Table 1
| Characteristics | Values |
|---|---|
| Age (years) | 59.6±15.5 |
| Male/female | 76/12 |
| Nutrition risk screening score | 2.65±1.36 |
| Tolerance for enteral nutrition score | 0.79±0.98 |
| Time of enteral nutrition (days) | 21 [7–25] |
| Death | 3 |
| Time of NJ tube catheterization (min) | 5.9±2.2 |
| Length of NJ tube insertion (cm) | 108.8±12.5 |
| Admission reason | |
| Severe pancreatitis | 6 (6.8) |
| Pneumonia | 5 (5.7) |
| Cerebrovascular disease | 13 (14.8) |
| Major operations | 60 (68.2) |
| Severe liver failure | 4 (4.5) |
Continuous data are presented as mean ± standard deviation. Time data are presented as mean [min–max]. Case data are shown as n (%). NJ, nasojejunal.
Improved endoscopically guided catheterization can significantly improve the nutritional status of patients
We evaluated the nutritional index data of patients receiving NJ tube EN before and after treatment. The results showed that after receiving 7 days of EN nutrition, the albumin level was significantly higher than that before intubation (36.42 vs. 33.66 g/L, P<0.001, Figure 2A), while the lymphocyte count, cholinesterase, and hemoglobin levels of the critically ill patients did not change significantly (Figure 2B-2D). This indicates that the improved endoscopically guided catheterization can meet the needs for improved nutrition status of patients while ensuring the depth and speed of NJ tube insertion.

Discussion
Malnutrition frequently manifests in critically ill patients (13). If left unaddressed over an extended period, malnutrition can exacerbate the primary disease and escalate mortality rates, significantly impacting the overall prognosis. However, timely nutritional intervention and support can substantially enhance the clinical outcomes of critically ill patients (1,12,14-16). In cases where patients are unable to consume food but have normal intestinal function, EN treatment is the preferred initial approach (17).
EN can be delivered through a nasogastric (NG) tube or an NJ tube. However, complications of upper gastrointestinal intolerance to EN have been reported in 31–46% of patients receiving NG feeding. Consequently, some prokinetic agents, such as metoclopramide and erythromycin, are used to enhance gastric motility and improve tolerance to enteral feeding. However, the specific preventive value of their usage and the optimal dosage of these drugs still require further exploration (18). In contrast, NJ feeding leads to fewer gastrointestinal complications, primarily achieved by reducing gastric residual volumes. As a result, the placement of an NJ feeding tube for providing energy support or medication is increasingly becoming a standard clinical practice for many patients (9,19,20).
Although the NJ tube is considered more effective and safer, its insertion requires a greater depth, making the procedure more intricate and demanding a higher level of expertise from endoscopists. Identifying safer and more efficient methods for tube insertion remains an urgent concern among clinical practitioners. Currently, several approaches, including the fluoroscopic technique, endoscopic technique, and guide wire technique, are utilized for NJ tube placement. The fluoroscopic method boasts a reported success rate of over 84%, while the endoscopically guided technique achieves an impressive success rate ranging between 90% and 100% (13,21-26). Recently, the invention of a wire-guided approach employing specialized traction wire devices has nearly achieved a remarkable 100% success rate, with an insertion time of merely 11 min, surpassing both the fluoroscopic method and endoscopic technique (9). However, the higher costs associated with patented equipment, such as guiding wires, limit its widespread adoption. In response, we have made improvements to the traditional endoscopically guided method. By adding a silk thread knot at the 25 cm mark from the end of the NJ tube and with the assistance of the physician using biopsy forceps through the gastroscope to hold the silk thread knot and aid in tube insertion, we achieved a significantly faster average insertion time of approximately 6 min. This greatly surpasses the conventional endoscopic placement speed (14 min) while ensuring effective insertion depth and reducing patient discomfort (17,27). Our modified insertion approach successfully improves the nutritional status of critically ill patients with the NJ tube placed, as evidenced by a notable recovery in serum albumin levels after 7 days of EN treatment, and the patients’ overall tolerance to the procedure is excellent.
The slight adjustments we made to the traditional endoscopic-guidance approach optimize both the time and depth of insertion, making it more cost-effective and easier for inexperienced physicians to master. This modified insertion method presents several advantages, including lower costs, extended and deeper tube retention, and reduced risks of aspiration and reflux. As a result, this technique emerges as a viable option for EN intervention in critically ill patients undergoing mechanical ventilation. However, our study was a retrospective study and had a limited number of participants enrolled. Subsequent research should focus on the practical application of the modified method in clinical settings and the timing of EN intervention, aiming to improve the prognosis of critically ill patients.
Conclusions
The improved endoscopically guided NJ tube placement technique is a rapid and safe procedure with excellent patient tolerance for critically ill patients. It significantly improves the nutritional status of critically ill patients and facilitates the administration of EN. The improved method needs further validation through randomized controlled trials.
Acknowledgments
Funding: This work was supported by Guangzhou Association for Science and Technology (No. K2023050111).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-87/rc
Data Sharing Statement: Available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-87/dss
Peer Review File: Available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-87/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-87/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Sun Yat-sen Memorial Hospital Ethics Committee (No. LX-HG-2023096) and conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent from participants was exempted due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Doley J. Enteral Nutrition Overview. Nutrients 2022;14:2180. [Crossref] [PubMed]
- Reintam Blaser A, Starkopf J, Alhazzani W, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med 2017;43:380-98. [Crossref] [PubMed]
- Liu M, Gao C. A systematic review and meta-analysis of the effect of total parenteral nutrition and enteral nutrition on the prognosis of patients with acute pancreatitis. Ann Palliat Med 2021;10:10779-88. [Crossref] [PubMed]
- Elke G, van Zanten AR, Lemieux M, et al. Enteral versus parenteral nutrition in critically ill patients: an updated systematic review and meta-analysis of randomized controlled trials. Crit Care 2016;20:117. [Crossref] [PubMed]
- Onuk S, Ozer NT, Savas N, et al. Enteral nutrition interruptions in critically ill patients: A prospective study on reasons, frequency and duration of interruptions of nutritional support during ICU stay. Clin Nutr ESPEN 2022;52:178-83. [Crossref] [PubMed]
- Slingerland-Boot R, Bouw-Ruiter M, van Manen C, et al. Video-assisted placement of enteral feeding tubes using the Integrated Real-Time Imaging System (IRIS)-technology in critically ill patients. Clin Nutr 2021;40:5000-7. [Crossref] [PubMed]
- Ling C, Hu X, Chen C, et al. Comparison of nutritional effectiveness and complication rate between early nasojejunal and nasogastric tube feeding in patients with an intracerebral hemorrhage. J Clin Neurosci 2022;103:107-11. [Crossref] [PubMed]
- Wang H, Huang C, Yang Y, et al. Cost-effectiveness analysis of nasojejunal tube feeding for the prevention of pneumonia in adults who are critically ill. JPEN J Parenter Enteral Nutr 2022;46:1167-75. [Crossref] [PubMed]
- Qin H, Lu XY, Zhao Q, et al. Evaluation of a new method for placing nasojejunal feeding tubes. World J Gastroenterol 2012;18:5295-9. [PubMed]
- Zhang Q, Sun JH, Liu JT, et al. Placement of a Jejunal Feeding Tube via an Ultrasound-Guided Antral Progressive Water Injection Method. Chin Med J (Engl) 2018;131:1680-5. [Crossref] [PubMed]
- Kolbeinsson HM, Veldkamp J, Paauw JD. Fluoroscopic placement of nasojejunal feeding tubes in COVID-19 patients in the prone position. JPEN J Parenter Enteral Nutr 2022;46:556-60. [Crossref] [PubMed]
- Taylor SJ, Karpasiti T, Milne D. Safety of blind versus guided feeding tube placement: Misplacement and pneumothorax risk. Intensive Crit Care Nurs 2023;76:103387. [Crossref] [PubMed]
- Tatsumi H, Akatsuka M, Kazuma S, et al. Endoscopic Insertion of Nasojejunal Feeding Tube at Bedside for Critically Ill Patients: Relationship between Tube Position and Intragastric Countercurrent of Contrast Medium. Ann Nutr Metab 2019;75:163-7. [Crossref] [PubMed]
- Lew CCH, Yandell R, Fraser RJL, et al. Association Between Malnutrition and Clinical Outcomes in the Intensive Care Unit: A Systematic Review JPEN J Parenter Enteral Nutr 2017;41:744-58. [Formula: see text]. [Crossref] [PubMed]
- Mogensen KM, Robinson MK, Casey JD, et al. Nutritional Status and Mortality in the Critically Ill. Crit Care Med 2015;43:2605-15. [Crossref] [PubMed]
- Hegde P, Chintanaboina J. Response to the author on "Percutaneous Ultrasound Gastrostomy (PUG) overview updates" in response to our review on "An overview of percutaneous endoscopic gastrostomy (PEG) tube placement in the intensive care unit (ICU)''. J Thorac Dis 2022;14:588-90. [Crossref] [PubMed]
- Alkhawaja S, Martin C, Butler RJ, et al. Post-pyloric versus gastric tube feeding for preventing pneumonia and improving nutritional outcomes in critically ill adults. Cochrane Database Syst Rev 2015;2015:CD008875. [Crossref] [PubMed]
- Gunn SR, Early BJ, Zenati MS, et al. Use of a nasal bridle prevents accidental nasoenteral feeding tube removal. JPEN J Parenter Enteral Nutr 2009;33:50-4. [Crossref] [PubMed]
- Jabłońska B, Mrowiec S. Nutritional Support in Patients with Severe Acute Pancreatitis-Current Standards. Nutrients 2021;13:1498. [Crossref] [PubMed]
- Chen Y, Tian X, Liu C, et al. Application of visual placement of a nasojejunal indwelling feeding tube in intensive care unit patients receiving mechanical ventilation. Front Med (Lausanne) 2022;9:1022815. [Crossref] [PubMed]
- Fan AC, Baron TH, Rumalla A, et al. Comparison of direct percutaneous endoscopic jejunostomy and PEG with jejunal extension. Gastrointest Endosc 2002;56:890-4. [Crossref] [PubMed]
- O'Keefe SJ, Foody W, Gill S. Transnasal endoscopic placement of feeding tubes in the intensive care unit. JPEN J Parenter Enteral Nutr 2003;27:349-54. [Crossref] [PubMed]
- Foote JA, Kemmeter PR, Prichard PA, et al. A randomized trial of endoscopic and fluoroscopic placement of postpyloric feeding tubes in critically ill patients. JPEN J Parenter Enteral Nutr 2004;28:154-7. [Crossref] [PubMed]
- Hu B, Ye H, Sun C, et al. Metoclopramide or domperidone improves post-pyloric placement of spiral nasojejunal tubes in critically ill patients: a prospective, multicenter, open-label, randomized, controlled clinical trial. Crit Care 2015;19:61. [Crossref] [PubMed]
- Kohata H, Okuda N, Nakataki E, et al. A novel method of post-pyloric feeding tube placement at bedside. J Crit Care 2013;28:1039-41. [Crossref] [PubMed]
- Lu G, Xiang Q, Wang S, et al. Endoscopic- versus x-ray-guidance for placement of nasojejunal tubes in critically ill patients: a systematic review and meta-analysis of randomized controlled trials. Am J Transl Res 2022;14:2134-46. [PubMed]
- Kurisawa K, Yokose M, Tanaka H, et al. Multivariate analysis of factors associated with first-pass success in blind placement of a post-pyloric feeding tube: a retrospective study. J Intensive Care 2021;9:59. [Crossref] [PubMed]
Cite this article as: Liang WL, Ma MZ, Min XH, Ouyang X, Liu J, Wu HH, Zhan CX, Li XM. Application and effectiveness of an improved endoscopically guided nasojejunal tube placement technique in critically ill patients: a retrospective cohort study. Transl Gastroenterol Hepatol 2023;8:36.