
History of colonoscopy and technological advances: a narrative review
Introduction
Colonoscopy plays a crucial role in the screening and treatment of colorectal cancer.
It is an optimal procedure for identifying precancerous polyps and recommended for screening individuals with risk factors, such as a family history of polyps or cancer (1). More than 15 million colonoscopies are performed in the United States yearly and it’s estimated to lower the overall risk of colorectal cancer death by more than 60% (2,3).
Colonoscopy first commenced in 1960s stemming from innovations in upper endoscopy (4). Gradual innovations into imaging technology, guideline developments, increased awareness led to increase in access and utility expansion.
Through this review, we will trace the origins exploring the historic perspectives and progression of colonoscopy, including awareness and guidelines, leading up to current practices and future advances including newer technologies in improving clinical success and expanding scope of colonoscopy. This review aims to provide holistic timeline celebrating various landmark achievements which have evolved the field of gastroenterology and expands to discuss promising future advances. We present the following article in accordance with the Narrative Review reporting checklist (available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-4/rc).
Methods
We utilized information from a variety of articles across major databases to write this narrative review including PubMed, Embase and Cochrane up to December 20, 2022 using key terms including but not limited to “colonoscopy”, “technological advancements”, “history” and “timeline” as shown in Table 1. Additional hand search was performed and in-text references of evaluated articles were also reviewed.
Table 1
| Items | Specification |
|---|---|
| Date of search | Databases searched up to December 20, 2022 |
| Databases and other sources searched | PubMed, Embase, Cochrane |
| Search terms used | Colonoscopy, Technological advancements, history, timeline |
| Timeframe | No specific time limitation was determined with aim to obtain most up to date information up to search date |
| Inclusion and exclusion criteria | No language restriction was applied |
| All relevant articles related to search terms were evaluated | |
| Exclusion criteria included abstracts, news articles, studies with statistical analysis, animal studies | |
| Selection process | Dr. Dahiya, Dr. Aziz and Dr. Nawras conducted data collection and consensus was obtained by Dr. Gangwani |
Origins and evolution to colonoscopy
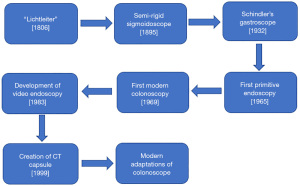
The advent of colonoscopy started off with the development of a primitive endoscope by Philipp Bozzini, who is considered to be the father of endoscopy (5). He created a rudimentary device, the Lichtleiter or “light conductor”, to examine the inner cavities of the human body (Figure 1). The device consisted of 2 parts, a hollow part from which light was emitted and reflected, using a fixed candle and mirror, and a mechanical part, designed to adapt to the body cavity needing to be examined for instance the ear, female bladder and urethra (6). He further emphasized utility of direct visualization for improving performance and safety of procedures, such as the removal of rectal polyps or cervical tumors to be done under direct visualization for optimal results considering safety and efficacy. This served as a baseline for future endoscopic inventions (5).

The first colonoscopy
Advances in colonoscopy proceeded by developments in sigmoidoscopy and innovations in upper endoscopic tools. Prior to that, simple anal and rectal specula examinations have been traced historically in Pompei ruins (7).
First sigmoidoscopy was performed in 1884 using a simple reflective lamp. It proceeded with creation of fiber-optic illumination system for improved visualization followed by flexible sigmoidoscope (8). These rigid sigmoidoscopes, depending on surgical expertise, could extend up to the splenic flexure but resulted in significant patient discomfort and were not preferred by surgeons (9). Rudolf Schindler, in the 1930s, conducted a series of experiments and developed the first semi-rigid gastroscope (6). Utilizing similar technology, Luciano Provenzale and Antonio Revignas, performed the first complete colonoscopy in Sardinia, Italy. They had a patient swallow a piece of vinyl tubing, which exited the anus and subsequently passed a gastroscope through the tube, that was pulled through to the colon all the way to the cecum (10). In 1969 at New York’s Beth Israel Medical Center, Wolff and Shinya performed one of the first modern colonoscopies. They utilized a colonoscope developed in Tokyo by Dr. Niwa and Dr. Yamagata. Additionally, Dr. Shinya developed a wire loop snare-cautery device that enabled the immediate removal of polyps, eliminating the need for a second redo procedure. They performed over 1,600 diagnostic procedures between June 1969 and June 1972 using a specially designed flexible fiberoptic instrument. This was a significant breakthrough in the early detection and treatment of colorectal cancer, and their protocol became the industry standard (11,12).
Current trends in colonoscopy
The modern colonoscope can suction, insufflate with air or water and biopsy with a shaft enhancing its utility greatly. Colonoscopies have undergone a dynamic technological shift, from their advent, starting off initially as rigid endoscopes and evolving into flexible endoscopes with snare capabilities and cautery mechanisms. In the 1980s and 1990s, colonoscopy as a procedure advanced, including the evolution of video endoscopy (13). Video endoscopy provided numerous benefits, most notably improved viewing of an enlarged image on a screen with both eyes at a convenient distance, simultaneous viewing by members of an entire team, and improved ergonomics for the endoscopist (14). Furthermore, the easy-to-capture images and video recordings improved documentation not only for medical but also for educational purposes. Since then, there have been subsequent improvements in visualization techniques, with devices improving not only the degree of visibility but the contrast, leading to improvement in adenoma detection rates (ADRs) and therefore improving colonoscopy yield.
At present, High definition-white light endoscopy (HD-WLE) is considered standard of care (15). There have been multiple newer modalities to further increase and enhance field of vision to aid, increase procedural technical stability and subsequently increase diagnostic yield (15). Figure 2 illustrates a historical timeline of events leading to modern day colonoscope.
Awareness
In the 20th century, even as colonoscopy continued to evolve, there remained limited awareness, generalizability or access towards colonoscopy with increased popularity of fecal occult blood testing or sigmoidoscopy. By 1999, according to a CDC (The Centers for Disease Control and Prevention) survey, only 40.3% American adults over age of 50 had ever had a sigmoidoscopy or colonoscopy. The number of colonoscopies performed increased significantly in the early 21st century (16).
In the United States, rate of colonoscopies more than doubled from 20% in 2000 to 47% in 2008 (17). Prior to the pandemic, approximately 68.8% of adults in the United States had a colonoscopy (17,18). A meta-analysis conducted by Zhang et al., demonstrated colonoscopy was associated with a 52% relative risk (RR) reduction in incidence of colorectal cancer (CRC) [RR: 0.48, 95% confidence interval (CI): 0.46–0.49] and 62% RR reduction in mortality of CRC (RR: 0.38, 95% CI: 0.36–0.40) (19).
Guidelines and quality control
By the mid-1990s, the United States had developed its first screening recommendations and a criterion was established, recommending colonoscopies to be performed on adults over age 50.
The American Society for Gastrointestinal Endoscopy (ASGE) issued the first colonoscopy guidelines in 2000 (20). This pioneered the establishment of quality indicators for screening colonoscopy for colorectal cancer detection and prevention to enhance colonoscopy quality and establish benchmarks for colonoscopy performance. The U.S. Multi-Society Task Force (USMSTF) first published a comprehensive list of quality indicators in 2002 with key indicators including ADR, adequate bowel preparation, cecal intubation rate, withdrawal time (21).
Overall, rates of colon cancer have declined, however between 2000 and 2015, colon cancer rates increased significantly among younger populations. Colorectal cancer incidence increased 28% in adults aged 40–44, 15% in adults aged 45–49, and 17% in adults aged 50–54, while colonoscopy rates increased 17% in adults aged 50–54 (22).
These recent changes, prompted initiatives such as the U.S. Preventive Services Task Force’s 2020 recommendation that all adults aged 45–75 be screened on a regular basis, updating the previous 2016 guidelines of screening at age 50 (23).
Technical advancements
There have been various technical advancements to further improve colonoscopy. More recently, there have been advancements in distal attachment devices such as endocuff vision, amplify EYE, G-EYE device, to optimize viewable mucosa and improve visual gaze. The endocuff device, helps flatten large mucosal folds, through its uniquely designed arms and helps improve visibility. A recently conducted meta-analysis has shown improved ADRs when comparing endocuff assisted colonoscopies to conventional colonoscopies (24). Similarly, G-EYE has a reusable balloon, allowing centralizing colonoscope optics, straightening folds and minimizing slippage (25).
Linked color imaging (LCI), a visualization process that helps improve the detection of adenomas, helps enhance color differences between mucosa and polyp tissue allowing for a higher chance of complete resection (26,27). A recent prospective randomized controlled trial comparing white-light imaging (WLI), blue-laser imaging (BLI) and LCI determined LCI had significant increase in ADR in screening colonoscopies (26).
Additionally, the development of virtual chromoendoscopy, which includes narrow-band imaging (NBI), Flexible Spectral Imaging Color Enhancement (FICE) and I-scan provides a method for electronic endoscopic imaging with improved contrast enhancement of mucosal surfaces and for image enhancement to help evaluate and assess depth of lesion (28).
Additional technical advances are under study to improve outcomes and lower discomfort. Colonoscopy techniques such as water immersion colonoscopy in comparison to air insufflation helps facilitate cecal intubation, reduce colonic distension and patient discomfort. These newer technical advances have utility with enhanced adenoma detection, mucosal resection and role in procedures such as sigmoid volvulus detorsion (29).
Artificial intelligence (AI) has a promising role in colonoscopy. AI can assist in colon cancer screening and classification of polyps. A recent network meta-analysis compared AI impact with other endoscopic interventions which suggested AI had statistically significant improvement of ADR compared to other interventions (30).
Expanding role of colonoscopy in interventions
Role of colonoscopy has expanded with technological advancements since the advent of colonoscopy. The first intervention in colonoscopy was in 1969 with polyp retrieval using wire loop snare-cautery device (12). Currently colonoscopy is also indicated as a therapeutic intervention for a number of gastrointestinal (GI) pathologies, such as localization and ablation of lower gastrointestinal bleeds, dilatation of colonic stenosis, management of large bowel perforation, foreign body removal and multiple other pathologies (31,32).
For lower GI bleeding, colonoscopies are the primary modality of treatment, with a wide variety of options being utilized, to achieve hemostasis, such as metal clip placement, thermal cauterization or an epinephrine injection. Depending on the etiology of treatment and cause of bleeding, studies report success rates as high 89% in achieving hemostasis with colonoscopic intervention (33).
Therapeutic colonoscopy also be used to treat acute obstructions including malignant colonic obstructions or strictures. It can be accomplished either by placing a self-expanding metal stent (SEMS), placement of a decompression tube or tumor debulking. Endoscopic placement of SEMS has found to have a higher clinical success rate, with lower complications, improved symptomatic relief and patient acceptance rate compared to its counterparts (34).
Similarly, pathologies such as pseudo-obstruction (Ogilvie syndrome) can be managed using colonoscopy. For patients with cecal or sigmoid volvulus, colonoscopies may provide an initial urgent treatment procedure however definitive surgical therapy may still be indicated (35).
Colonic stenosis can also be treated with a colonoscopic procedure using either balloon dilation or electro-incision. Certain studies have reported a high success rate with a low complication rate, however recurrence is common (36).
Furthermore, there is expanding role of endomucosal resection (EMR) for large polyps to reduce the risk of delayed bleeding or perforation (37).
Conclusions
The colonoscope has evolved over time to become one of the most powerful tools utilized for screening, diagnostics and therapeutic interventions. It has had a remarkable progress in terms of acceptability, screening practices formalization of being included in guidelines and practice principles. Despite its aggregated success of improved visualization techniques and improved engineering design which has tremendously helped improved ADRs and enhanced scope of colonoscope, there remain limitations and remain room to further improve ADRs, improve patient comfort, detect neoplastic lesions using advanced imaging techniques and reduce adverse events. Adaptation of newer technological principles and tools in complementation with AI, can serve to further reduce the limitations and expand role of colonoscopy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Translational Gastroenterology and Hepatology for the series “Colonoscopy: Updates and Prospects”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-4/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tgh.amegroups.com/article/view/10.21037/tgh-23-4/coif). The series “Colonoscopy: Updates and Prospects” was commissioned by the editorial office without any funding or sponsorship. MA served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Translational Gastroenterology and Hepatology from September 2022 to August 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roy PS, Saikia BJ. Cancer and cure: A critical analysis. Indian J Cancer 2016;53:441-2. [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70:7-30. [Crossref] [PubMed]
- Pan J, Xin L, Ma YF, et al. Colonoscopy Reduces Colorectal Cancer Incidence and Mortality in Patients With Non-Malignant Findings: A Meta-Analysis. Am J Gastroenterol 2016;111:355-65. [Crossref] [PubMed]
- Hayman CV, Vyas D. Screening colonoscopy: The present and the future. World J Gastroenterol 2021;27:233-9. [Crossref] [PubMed]
- Ramai D, Zakhia K, Etienne D, et al. Philipp Bozzini (1773-1809): The earliest description of endoscopy. J Med Biogr 2018;26:137-41. [Crossref] [PubMed]
- Natalin RA, Landman J. Where next for the endoscope? Nat Rev Urol 2009;6:622-8. [Crossref] [PubMed]
- Edmonson JM. History of the instruments for gastrointestinal endoscopy. Gastrointest Endosc 1991;37:S27-56. [Crossref] [PubMed]
- Kaunitz JD. The fruits of fiber: the invention of the flexible fiberoptic gastroscope. Dig Dis Sci 2014;59:2616-8. [Crossref] [PubMed]
- Winawer SJ. The history of colorectal cancer screening: a personal perspective. Dig Dis Sci 2015;60:596-608. [Crossref] [PubMed]
- Fox JA, Provenzale L, Revignas A. Fibreoptic colonoscopy. Lancet 1970;1:107. [Crossref] [PubMed]
- Wolff WI, Shinya H. Colonofiberoscopy. JAMA 1971;217:1509-12. [Crossref] [PubMed]
- Lee A, Tutticci N. Enhancing polyp detection: technological advances in colonoscopy imaging. Transl Gastroenterol Hepatol 2021;6:61. [Crossref] [PubMed]
- Brown GJ, Saunders BP. Advances in colonic imaging: technical improvements in colonoscopy. Eur J Gastroenterol Hepatol 2005;17:785-92. [Crossref] [PubMed]
- Shergill AK, McQuaid KR, Rempel D. Ergonomics and GI endoscopy. Gastrointest Endosc 2009;70:145-53. [Crossref] [PubMed]
- Tziatzios G, Gkolfakis P, Lazaridis LD, et al. High-definition colonoscopy for improving adenoma detection: a systematic review and meta-analysis of randomized controlled studies. Gastrointest Endosc 2020;91:1027-36.e9. [Crossref] [PubMed]
- Trends in screening for colorectal cancer--United States, 1997 and 1999. MMWR Morb Mortal Wkly Rep 2001;50:162-6. [PubMed]
- Fedewa SA, Siegel RL, Jemal A. Are temporal trends in colonoscopy among young adults concordant with colorectal cancer incidence? J Med Screen 2019;26:179-85. [Crossref] [PubMed]
- Amlani B, Radaelli F, Bhandari P. A survey on colonoscopy shows poor understanding of its protective value and widespread misconceptions across Europe. PLoS One 2020;15:e0233490. [Crossref] [PubMed]
- Zhang J, Chen G, Li Z, et al. Colonoscopic screening is associated with reduced Colorectal Cancer incidence and mortality: a systematic review and meta-analysis. J Cancer 2020;11:5953-70. [Crossref] [PubMed]
- Minoli G, Meucci G, Bortoli A, et al. The ASGE guidelines for the appropriate use of colonoscopy in an open access system. Gastrointest Endosc 2000;52:39-44. [Crossref] [PubMed]
- Rex DK, Bond JH, Winawer S, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2002;97:1296-308. [Crossref] [PubMed]
- Crosbie AB, Roche LM, Johnson LM, et al. Trends in colorectal cancer incidence among younger adults-Disparities by age, sex, race, ethnicity, and subsite. Cancer Med 2018;7:4077-86. [Crossref] [PubMed]
- Davidson KW, Barry MJ, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2021;325:1965-77. [Crossref] [PubMed]
- Aziz M, Haghbin H, Gangwani MK, et al. Efficacy of Endocuff Vision compared to first-generation Endocuff in adenoma detection rate and polyp detection rate in high-definition colonoscopy: a systematic review and network meta-analysis. Endosc Int Open 2021;9:E41-50. [Crossref] [PubMed]
- Shirin H, Shpak B, Epshtein J, et al. G-EYE colonoscopy is superior to standard colonoscopy for increasing adenoma detection rate: an international randomized controlled trial (with videos). Gastrointest Endosc 2019;89:545-53. [Crossref] [PubMed]
- Dos Santos CEO, Malaman D, Arciniegas Sanmartin ID, et al. Effect of Linked-color Imaging on the Detection of Adenomas in Screening Colonoscopies. J Clin Gastroenterol 2022;56:e268-72. [Crossref] [PubMed]
- Suzuki T, Hara T, Kitagawa Y, et al. Linked-color imaging improves endoscopic visibility of colorectal nongranular flat lesions. Gastrointest Endosc 2017;86:692-7. [Crossref] [PubMed]
- Pal P, Singh AP, Kanuri ND, et al. Electronic chromo-endoscopy: technical details and a clinical perspective. Transl Gastroenterol Hepatol 2022;7:6. [Crossref] [PubMed]
- Sugimoto S, Mizukami T. Diagnostic and therapeutic applications of water-immersion colonoscopy. World J Gastroenterol 2015;21:6451-9. [Crossref] [PubMed]
- Aziz M, Haghbin H, Sayeh W, et al. Comparison of Artificial Intelligence With Other Interventions to Improve Adenoma Detection Rate for Colonoscopy: A Network Meta-analysis. J Clin Gastroenterol 2022; Epub ahead of print. [Crossref] [PubMed]
- Hammami A, Elloumi H, Bouali R, et al. Clinical practice standards for colonoscopy. Tunis Med 2021;99:952-60. [PubMed]
- Serur A, Rhee R, Ramjist J. Current Nonoperative Therapeutic Interventions for Lower Gastrointestinal Hemorrhage. Clin Colon Rectal Surg 2020;33:22-7. [Crossref] [PubMed]
- Sagar J. Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev 2011;2011:CD007378. [Crossref] [PubMed]
- Saunders MD. Acute colonic pseudo-obstruction. Best Pract Res Clin Gastroenterol 2007;21:671-87. [Crossref] [PubMed]
- Hassan C, Zullo A, De Francesco V, et al. Systematic review: Endoscopic dilatation in Crohn's disease. Aliment Pharmacol Ther 2007;26:1457-64. [Crossref] [PubMed]
- Koornstra JJ, Weersma RK. Management of rectal foreign bodies: description of a new technique and clinical practice guidelines. World J Gastroenterol 2008;14:4403-6. [Crossref] [PubMed]
- van Hattem WA, Shahidi N, Vosko S, et al. Piecemeal cold snare polypectomy versus conventional endoscopic mucosal resection for large sessile serrated lesions: a retrospective comparison across two successive periods. Gut 2021;70:1691-7. [Crossref] [PubMed]
Cite this article as: Gangwani MK, Aziz A, Dahiya DS, Nawras M, Aziz M, Inamdar S. History of colonoscopy and technological advances: a narrative review. Transl Gastroenterol Hepatol 2023;8:18.


