
Treatment of ileal Dieulafoy’s lesion by hemostatic clips under double-balloon enteroscopy: a case report
Introduction
Dieulafoy’s lesion (DL) is a developmental vascular malformation of the gastrointestinal tract, which was firstly described by a French surgeon in 1898 (1). The diameter of the lesion’s artery, which ranges 1–3 mm, is almost 10 times that of normal arteries at the muscularis mucosae level, which may increase the risk of massive bleeding (2). The most common site of DL is the stomach, accounting for nearly three quarters, and the rarest site is the small intestine, only accounting for 1% (3). Herein, we reported a case with DL in ileum, which was then successfully treated by hemostatic clips under double-balloon enteroscopy (DBE). We present the following case in accordance with the CARE reporting checklist (available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-14/rc).
Case presentation
On August 24, 2021, a 66-year-old female underwent endoscopy at outpatient department of our hospital due to hematochezia and abdominal distension and pain for more than 10 days. Gastroduodenoscopy did not find any sign of bleeding. Colonoscopy showed large blood clots in the intestinal tract, but did not detect any bleeding lesion. On August 28, 2021, she was admitted to the Department of General Surgery of our hospital. She had a history of diabetes, hypertension, coronary heart disease, atrial fibrillation, and mitral insufficiency, and a recent diagnosis of acute cerebral infarction for 10 days. And she had a medication history of aspirin, but aspirin had been stopped three months before this admission. Laboratory examinations showed hemoglobin (HGB) 71 g/L (reference range, 130–175 g/L), red blood cells (RBC) 2.44×1012/L (reference range, 4.3–5.8×1012/L), prothrombin time (PT) 15.1 s (reference range, 11.0–14.3 s), fibrinogen (FIB) 1.88 g/L (reference range, 2.00–4.00 g/L), antithrombin III (AT III) 69% (reference range, 80–120%), and D-dimer 1.54 µg/mL (reference range, 0.00–0.50 µg/mL). After pharmacological hemostasis, blood transfusion, and intravenous fluid supplementation, an angiogram was performed, but no source of bleeding was accurately identified.
On August 29, 2021, she was transferred to our department. After conservative therapy, HGB became up to 83 g/L. Considering that she had a recent history of acute cerebral infarction with coronary artery stenosis, a more invasive diagnostic approach, including DBE on general anesthesia, was compromised.
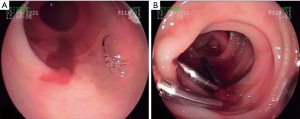
On August 31, 2021, the patient still presented with hematochezia. HGB was decreased to 66 g/L. Thus, a capsule endoscopy was performed and suggested that bleeding may be located in ileum. DBE via anal route was performed by an experienced endoscopist (F Gao), and showed active pulsatile bleeding in the upper part of ileum, without underlying ulcer, but with normal mucosa around the small defected mucosal lesions, which is consistent with a diagnosis of DL (Figure 1A). Then, 3 hemostatic clips were locally placed and 25,000 U thrombin was sprayed on the lesion to effectively treat this disease (Figure 1B). Finally, bleeding stopped.
The patient did not develop hematochezia after endoscopic treatment. On September 9, 2021, HGB was 94 g/L. The patient was discharged without any recurrence of gastrointestinal bleeding at a 4-month follow-up.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
DL, a rare cause of life-threatening gastrointestinal bleeding, constitutes about 1% to 2% of all episodes of gastrointestinal bleeding (1). In adults, the prevalence of DL in male versus female is 2:1 (4). In addition, DL can be found in all age groups, especially in the elderly with multiple comorbidities, such as cardiovascular disease, hypertension, chronic kidney disease, and diabetes mellitus (5). Notably, multiple comorbidities were found in our patient.
Our patient presented with hematochezia. Initially, some possible causes for hematochezia were considered, mainly including diverticular bleeding, telangiectasias, vascular neoplasms, colitis, and malignancy. Finally, small bowel was considered as the potential location of bleeding in our patient. According to the clinical guidelines (6), patients with suspected small bowel bleeding should repeat gastroduodenoscopy or colonoscopy, if necessary. Meanwhile, hemodynamically stable patients with active bleeding can undergo computed tomography angiography (CTA) to identify the site of bleeding. Unfortunately, in our patient, conventional diagnostic approaches, including gastroduodenoscopy, colonoscopy, and even angiogram, did not show any definite bleeding source of gastrointestinal bleeding. Clinical guideline also recommends that video capsule endoscopy (VCE) should be firstly considered, if second-look gastroduodenoscopy and colonoscopy examinations are negative, and that computed tomographic enterography (CTE) or magnetic resonance (MR) should be performed in patients with suspected small bowel stenosis and negative capsule endoscopy (6). If CTE, MR, or VCE examinations are positive, deep enteroscopy should be further performed (6). In our patient, DBE via anal route was performed under the guidance of capsule endoscopy, and then showed that the location of bleeding should be ileum. Except for the approaches mentioned above, other advanced diagnostic approaches for detecting DL in small intestine were also employed in previous literature, including laparotomy, technetium-99m-labelled red blood cell scan (Tc99mRBCs), and ileoscopy (Table 1) (7-31).
Table 1
| First author (year) | Region | Number of patients | Sex (male/female) | Age, years | Symptoms | Comorbidities | Approaches for detecting lesions | Lesion location | Treatment | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| Arai (2021) | Japan | 1 | M | 66 | Tarry stool | Cardiovascular disease and diabetes | Capsule endoscopy | Small intestine | APC | Alive 18 months |
| Wang (2021) | China | 1 | M | 7 | Melena | Hypertension | Enteroscopy | Jejunum | Surgery | Alive 12 months |
| Salimi (2021) | Iran | 1 | M | 68 | Hematemesis | No | CTA | Small intestine | Surgery | Alive 36 months |
| Saada (2019) | Israel | 1 | M | 27 | Bloody diarrhea | NA | Tc99mRBCs and Laparotomy | Jejunum | Surgery | Alive 3 months |
| Kawabata (2019) | Japan | 1 | M | 81 | Tarry stool | Cerebral infarction | Enhanced CT and Enteroscopy | Jejunum | Hemoclips | Death unrelated to DL 10 weeks |
| Kieswetter (2019) | Canada | 1 | F | 9 | Melena and fresh blood | No | Angiography and enteroscopy | Jejunum | Surgery | Alive 48 months |
| Jung (2019) | Germany | 1 | NA | 69 | Melena | No | Enteroscopy | Jejunum | OTSC clip | Alive 6 days |
| Zhao (2018) | China | 1 | M | 41 | Hematochezia | NA | Enteroscopy | Jejunum | Surgery | Alive 6 months |
| Becq (2018) | France | 1 | F | 32 | Hematochezia | No | CTA and endoscopy | Ileum | Surgery | NA |
| Seo (2017) | Korea | 1 | M | 25 | Hematochezia | No | Angiography and capsule endoscopy | Jejunum | Surgery | Alive 24 months |
| Chen (2016) | China Taiwan | 1 | M | 54 | Bloody stool | Hypertension | Enteroscopy and CTA | Ileum | Hemoclips and surgery | Alive 3 months |
| Ego (2015) | Japan | 1 | F | 95 | Melena | Chronic cardiac failure and chronic kidney disease | Enteroscopy | Jejunum | Endoscopic band ligation | Alive 1 month |
| Shibutani (2011) | Japan | 1 | F | 14 | Hematochezia | No | CT scan and angiography | Ileum | Surgery | NA |
| Saji (2010) | Japan | 1 | M | 72 | Melena | Hypertension | Angiography, CT scan, and gastrointestinal endoscopy | Jejunum | Epinephrine injection and hemoclips | NA |
| Moreira-Pinto (2009) | Portugal | 1 | F | 14 | Hematochezia | NA | Laparotomy | Jejunum | Surgery | Alive 48 months |
| Yano (2008) | Japan | 6 | M | 58 | NA | NA | Enteroscopy | Jejunum | APC | NA |
| M | 68 | NA | NA | Enteroscopy | Jejunum | APC and epinephrine injection | NA | |||
| F | 72 | NA | NA | Enteroscopy | Jejunum | Hemoclips | NA | |||
| M | 56 | NA | NA | Enteroscopy | Jejunum | Hemoclips | NA | |||
| F | 71 | NA | NA | Enteroscopy | Ileum | Hemoclips | NA | |||
| M | 24 | NA | NA | Enteroscopy | Jejunum | Surgery | NA | |||
| Tsai (2007) | China Taiwan | 1 | M | 2 | Dark-red stool | NA | Angiography | Ileum | Surgery | NA |
| Palma (2006) | Italy | 1 | M | 50 | Melena | Cardiovascular disease | Capsule endoscopy and enteroscopy | Small intestine | Hemoclips | Alive 6 months |
| Kim (2005) | Korea | 1 | M | 35 | Dizziness and palpitation | NA | CT scan | Jejunum | Surgery | NA |
| Mino (2004) | Japan | 1 | F | 31 | Melena | NA | Tc99mRBCs and angiography | Jejunum | Surgery | Alive 36 months |
| Morowitz (2004) | America | 1 | M | 4 | Hematochezia | No | Laparotomy | Ileum | Surgery | NA |
| Iglesias (2004) | Spain | 1 | M | 68 | Rectal bleeding | NA | Ileoscopy | Ileum | Hemoclips and epinephrine injection | Alive 12 months |
| Fox (2001) | Britain | 1 | F | 47 | Melaena | Hypertension | Laparotomy | Ileum | Surgery | NA |
| Blecker (2001) | America | 2 | M | 18 | Maroon colored stool | No | Tc99mRBCs and laparotomy | Jejunum | Surgery | NA |
| F | 69 | Abdominal pain | Peptic ulcer disease |
Enteroscopy and laparotomy | Ileum | Surgery | NA | |||
| Lee (1997) | Korea | 1 | F | 20 | Hematochezia | NA | Tc99mRBCs | Jejunum | Surgery | Alive 2 months |
DL, Dieulafoy’s lesion; APC, argon plasma coagulation; OTSC, over-the-scope; CT, computed tomography; CTA, computed tomography angiography; Tc99mRBCs, technetium-99m-labelled red blood cell scan; NA, not applicable.
Until now, there is no available consensus regarding the treatment of DL. The treatment approaches for DL mainly include endoscopic and surgical treatments. Of the DL located in the upper gastrointestinal tract, 85% can be successfully treated by endoscopic therapy, and only 5% require surgery (32). However, it is difficult to detect DL located in the lower gastrointestinal tract, especially jejunum and ileum, by endoscopies, primarily due to residual stool and massive bleeding resulting in poor visualization of the gastrointestinal tract. Therefore, surgery is the preferred choice to treat small intestinal DL. Indeed, based on previous case reports (Table 1), surgery has been the most commonly used treatment approach for DL located in small intestine, but other approaches that are less invasive can be effective for the treatment of small intestinal DL. Approaches of endoscopic hemostasis mainly include mechanical hemostasis (i.e., hemostatic clips and endoscopic band ligation), regional injection (i.e., regional injection-epinephrine or norepinephrine injection and sclerotherapy), and argon plasma coagulation (APC) (1). In our patient, hemostatic clips were locally placed on the lesion to effectively treat ileal DL, which avoided surgery. In addition, angiography can be used to control bleeding by selective embolization of the feeding vessel (2).
Follow-up duration after successful treatment is heterogeneous among previous studies (Table 1), but no recurrence of DL is reported. Similarly, no recurrence after endoscopic treatment was observed in our case during a 4-month follow-up. Certainly, it is very necessary to monitor the risk of recurrent bleeding during the long-term follow-up in the future.
In conclusion, small intestinal DL is rare and difficult to be detected by conventional approaches. Notably, DBE is an effective diagnostic approach for DL in small intestine. Endoscopic treatment should be considered as a preferred choice of treatment with less invasiveness and lower cost as compared to surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-14/rc
Peer Review File: Available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-14/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-14/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Malik TF, Anjum F. Dieulafoys Lesion Causing Gastrointestinal Bleeding. [Updated 2021 Dec 8]. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2022.
- Lee YT, Walmsley RS, Leong RW, et al. Dieulafoy's lesion. Gastrointest Endosc 2003;58:236-43. [Crossref] [PubMed]
- Marangoni G, Cresswell AB, Faraj W, et al. An uncommon cause of life-threatening gastrointestinal bleeding: 2 synchronous Dieulafoy lesions. J Pediatr Surg 2009;44:441-3. [Crossref] [PubMed]
- Baxter M, Aly EH. Dieulafoy's lesion: current trends in diagnosis and management. Ann R Coll Surg Engl 2010;92:548-54. [Crossref] [PubMed]
- Saleh R, Lucerna A, Espinosa J, et al. Dieulafoy lesion: the little known sleeping giant of gastrointestinal bleeds. Am J Emerg Med 2016;34:2464.e3-5. [Crossref] [PubMed]
- Gerson LB, Fidler JL, Cave DR, et al. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol 2015;110:1265-87; quiz 1288. [Crossref] [PubMed]
- Arai Y, Ogawa M, Arimoto R, et al. Contribution of Capsule Endoscopy Early in a Bleeding Episode to Treatment of Small Bowel Angioectasia: A Case Report. Medicina (Kaunas) 2021;57:321. [Crossref] [PubMed]
- Wang M, Cao H, Dai J, et al. Jejunal Dieulafoy lesion with intraintestinal calcification on computerized tomography: A case report. Medicine (Baltimore) 2021;100:e26229. [Crossref] [PubMed]
- Salimi J, Behzadi M, Ramandi A, et al. Chronic gastrointestinal bleeding caused by a Dieulafoy's lesion in the small intestine: a case report. J Med Case Rep 2021;15:545. [Crossref] [PubMed]
- Saada M, Perek S, Agbaria M, et al. Massive Gastrointestinal Bleeding from a Jejunal Dieulafoy Lesion: An Extraordinary Presentation. Case Rep Gastroenterol 2019;13:508-13. [Crossref] [PubMed]
- Kawabata H, Kawakatsu Y, Sone D, et al. A rare case of Goodpasture syndrome concomitant with bleeding jejunal Dieulafoy's lesion. Clin J Gastroenterol 2020;13:382-5. [Crossref] [PubMed]
- Kieswetter L, Walters TD, Lara-Corrales I, et al. Dieulafoy lesions and PHACE syndrome. Pediatr Dermatol 2019;36:902-5. [Crossref] [PubMed]
- Jung C, Kunsch S, Bremer S, et al. Colonoscopy-assisted application of a 14/6t over-the-scope clip for treatment of a bleeding Dieulafoy lesion in the distal jejunum. Endoscopy 2019;51:E92-3. [Crossref] [PubMed]
- Zhao J, Sun Z, Zhang X. A Jejunal Dieulafoy's Lesion Mimicking a Gastrointestinal Stromal Tumor. Clin Gastroenterol Hepatol 2019;17:A19. [Crossref] [PubMed]
- Becq A, Dray X, Boarini G. Massive Ileal Bleeding Secondary to a Dieulafoy's lesion. Endosc Int Open 2018;6:E495-7. [Crossref] [PubMed]
- Seo KI, Moon W, Lee CW, et al. Minimal Resection of Jejuna Dieulafoy's Lesion Using an Intraoperative Fluoroscopic Localization of the Metallic Coils Used in Angiography. Korean J Gastroenterol 2017;69:135-8. [Crossref] [PubMed]
- Chen IS, Chuang HW, Tai CM. Gastrointestinal: Ileal Dieulafoy's lesion presenting as a bleeding submucosal tumor. J Gastroenterol Hepatol 2016;31:1914. [Crossref] [PubMed]
- Ego M, Shimamura Y, Ishii N. Endoscopic band ligation with double-balloon endoscopy for treatment of jejunal Dieulafoy's lesion. Dig Endosc 2015;27:627. [Crossref] [PubMed]
- Shibutani S, Obara H, Ono S, et al. Dieulafoy lesion in the ileum of a child: a case report. J Pediatr Surg 2011;46:e17-9. [Crossref] [PubMed]
- Saji N, Yoda J, Tadano M, et al. Elderly case of Dieulafoy's lesion in the jejunum presenting with repeated hemorrhagic shocks. Geriatr Gerontol Int 2010;10:267-8. [Crossref] [PubMed]
- Moreira-Pinto J, Raposo C, Teixeira da Silva V, et al. Jejunal Dieulafoy's lesion: case report and literature review. Pediatr Surg Int 2009;25:641-2. [Crossref] [PubMed]
- Yano T, Yamamoto H, Sunada K, et al. Endoscopic classification of vascular lesions of the small intestine (with videos). Gastrointest Endosc 2008;67:169-72. [Crossref] [PubMed]
- Tsai CL, Yang MC, Cheng KC, et al. Ileal Dieulafoy's lesion with massive hematochezia. J Am Coll Surg 2007;204:710. [Crossref] [PubMed]
- De Palma GD, Patrone F, Rega M, et al. Actively bleeding Dieulafoy's lesion of the small bowel identified by capsule endoscopy and treated by push enteroscopy. World J Gastroenterol 2006;12:3936-7. [Crossref] [PubMed]
- Kim JK, Jo BJ, Lee KM, et al. Dieulafoy's lesion of jejunum: presenting small bowel mass and stricture. Yonsei Med J 2005;46:445-7. [Crossref] [PubMed]
- Mino A, Ogawa Y, Ishikawa T, et al. Dieulafoy's vascular malformation of the jejunum: first case report of laparoscopic treatment. J Gastroenterol 2004;39:375-8. [Crossref] [PubMed]
- Morowitz MJ, Markowitz R, Kamath BM, et al. Dieulafoy's lesion and segmental dilatation of the small bowel: an uncommon cause of gastrointestinal bleeding. J Pediatr Surg 2004;39:1726-8. [Crossref] [PubMed]
- Iglesias SS, Rosés LL, Ramrez AG, et al. Ileal Dieulafoy's lesion. Gastrointest Endosc 2004;59:266. [Crossref] [PubMed]
- Fox A, Ravi K, Leeder PC, et al. Adult small bowel Dieulafoy lesion. Postgrad Med J 2001;77:783-4. [Crossref] [PubMed]
- Blecker D, Bansal M, Zimmerman RL, et al. Dieulafoy's lesion of the small bowel causing massive gastrointestinal bleeding: two case reports and literature review. Am J Gastroenterol 2001;96:902-5. [Crossref] [PubMed]
- Lee KS, Moon YJ, Lee SI, et al. A case of bleeding from the Dieulafoy lesion of the jejunum. Yonsei Med J 1997;38:240-4. [Crossref] [PubMed]
- Akhras J, Patel P, Tobi M. Dieulafoy's lesion-like bleeding: an underrecognized cause of upper gastrointestinal hemorrhage in patients with advanced liver disease. Dig Dis Sci 2007;52:722-6. [Crossref] [PubMed]
Cite this article as: Gao C, Guo X, Li H, Chen H, Gao Z, Gao F, Qi X. Treatment of ileal Dieulafoy’s lesion by hemostatic clips under double-balloon enteroscopy: a case report. Transl Gastroenterol Hepatol 2023;8:21.


