Complete mesocolic excision for colon cancer is technically challenging but the most oncological appealing
Introduction
We read with really great interest the paper published by Gao et al. in Annals of Surgery (1). The authors presented the 3-year interim results of the Efficacy Study of Complete Mesocolic Excision, which is a prospective, non-randomized study with a planned duration of 5 years, started in 2012 (1). The main objective of this study is to evaluate the safety and effectiveness of complete mesocolic excision for colon cancer treatment. Gao et al. included 220 and 110 patients in the CME and conventional surgery groups, respectively. An important strength of the current study is the evaluation of the specimens by blinded third-party experts (1).
Complete mesocolic excision with central vascular ligation (CME-CVL) for colon cancer represents nothing more than reiteration of the most classical principles of surgical oncology, such as accurate tissue dissection, following embryological planes, with ligation of the feeding arteries at their origin (2,3). The CME-CVL, which follows the same principles as total mesorectal excision for rectal cancer, was proposed by Hohenberger et al.; the group from Erlangen Germany reported a reduction in local 5-year recurrences from 6.5% to 3.6%, with increasing in the cancer related 5-year survival rate from 82.1% to 89.1% (4). The current evidence shows that CME-CVL offers better resected specimens, with higher mesenteric area, higher distance tumor to high tie, and higher number of resected lymph nodes (5,6). However, there is an ongoing debate in the literature regarding the benefit/risk ratio for CME-CVL technique, with contradictory long-term oncological results of two recent systematic reviews (7,8). Alhassan et al. meta-analyzed the results of 14 studies, with 1,166 and 945 patients in the CME-CVL and non-CME groups, respectively (8). The overall complication rate in the CME and non-CME groups was 22.5% and 19.6%, with no differences for anastomotic leakage rates. The CME group was associated with a lower local recurrence rate in two studies and a better DFS in three out of 14 studies (8).
Methods
We performed an electronic literature search about the current topic in PubMed/Medline and Google Scholar databases. The search strategy used in PubMed was: ((colon cancer) AND ((complete mesocolic excision[Title/Abstract]) OR D3 lymphadenectomy[Title/Abstract])) (see Table 1).

Full table
Oncological outcomes
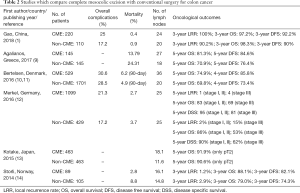
The long-term oncological outcomes of studies comparing CME with conventional colonic resections are summarized in Table 2. Gao et al. found a statistically significant lower local recurrence rate in the CME group (100% vs. 90.2%, P<0.001), with no differences regarding 3-year overall survival (OS), disease free survival (DFS) or metastasis free survival (MFS) survival (1). An et al. compared the oncological outcomes in 34 patients from laparoscopic CME group with 81 patients from non-CME group (15). CME group presented more retrieved lymph nodes (P<0.001) and less blood loss (P=0.016). Although there were no differences regarding 5-year DFS, the 5-year OS was 100% and 89.5% in the CME and non-CME groups, respectively (P<0.05) (15). Another study, comparing 97 CME and 95 non-CME patients, showed a 3-year OS of 88% compared to 71% (P=0.003); with a 3-year DSS of 97% vs. 86% for stage II; and 86% versus 67% for stage III patients (16).
Full table
Perioperative outcomes
In terms of perioperative outcomes, the study coming from Peking University People’s Hospital Beijing revealed no differences for postoperative complication rate, with less intraoperative blood loss and one day shorter hospital stay for the CME patients (see Table 2) (1).
Analysis of the short-term postoperative adverse outcomes from the Swedish Colorectal Cancer Registry revealed a proportion of CME resections of 14.8% in the 90-day reoperation or mortality group vs. 19.5% in the control group (17). The odds ratio for short-term mortality or reoperation after CME was 0.82 (95% CI, 0.47–1.10, P=0.15), with lower values in the later part of the study and high-volume centers (17). Analysis of a consecutive patients series after the introduction of CME technique revealed a complication rate of 47%, with severe complications (grade III and IV Clavien Dindo) in 15% of cases (18). Zurleni et al. published their cohort study with historical controls and showed a postoperative complication rate of 21.6% in CME and 17.8% in the non-CME group (P>0.05) (16).
Bertelsen et al. showed that CME for right-sided tumors is associated, in long-term evaluation, neither with bowel dysfunction nor lower quality of life (19). Evaluating 762 patients the authors revealed that CME was not associated with increased diarrhea (OR =1.07, P=0.84) or lower score on QLQ-C30 questionnaire (OR =0.84, P=0.50) (19).
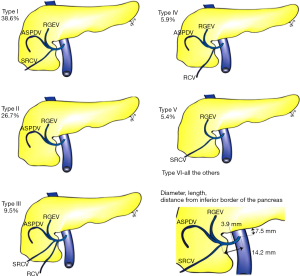
Although oncologically appealing, the CME-CVL is a technically demanding technique and requires a thorough understanding of the complex tridimensional vascular anatomy inside the base of the mesentery and mesocolon (20) (see Figure 1). A recent meta-analysis of 45 studies, with 6,090 specimens, revealed a prevalence of the ileocolic, right colic and middle colic arteries of 99.8%, 60.1% and 94.6%, respectively (20). Based on a pooled prevalence from this large dataset, a standardized terminology of the Henle trunk, present in 89.7% of cases, was proposed (20) (see Figure 2). The meta-analysis of 78 studies including 18,369 specimens showed that the first jejunopancreatic vein, which has as affluents the inferior pancreaticoduodenal and a variable number of jejunal veins, has a mean diameter of 5.37 mm and a trajectory anterior to the superior mesenteric artery in 28.2% (3).

Quality of the resected specimen
Regarding the resected specimen, the laparoscopic approach offers the same quality as the open approach in CME-CVL: retrieved lymph nodes [mean difference (MD) =−1.06, P=0.42] and tumor to high tie distance (MD =14.26 cm, P=0.13); the surface of the resected mesocolon was higher in the laparoscopic CME (MD =11.75 cm2, P<0.001) (21). On the other hand, laparoscopy is superior in all perioperative outcomes and at least non-inferior in long-term oncological outcomes (21). In the study of Gao et al., the CME resected specimen presented a higher number of resected lymph nodes (24 vs. 20, P=0.002), and all the morphometric data of the resected specimen, such as area of the mesentery (right colon: 13,052 vs. 9,093 mm2; sigmoid colon: 10,317 vs. 7475 mm2) and tumor to high tie distance (right colon: 129 vs. 113 cm; sigmoid colon: 143 vs. 121 cm), favoring CME (1) (see Table 2). Olofsson et al. investigated the clinical data for ceacum and ascending colon tumors, from Swedish Colorectal Cancer Registry, related to oncological impact of central ligation of (I) ileocolic +/− right colic vessels (390 patients); (II) ileocolic and right branch of the middle colic (1,360 patients); and (III) ileocolic and middle colic vessels (334 patients) (22). There were no differences regarding 3-year OS, 3-year DFS, and local recurrence rate, with an increase of perioperative mortality from 0.8% to 3.6% with extended resections (P=0.025) (22).
Conclusions
The complete mesocolic excision with central vascular ligation for colon cancer offers better quality of the resected specimens. The oncological outcomes seem to be superior and not counterbalanced by an increased morbidity for surgeons with appropriate training.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gao Z, Wang C, Cui Y, et al. Efficacy and Safety of Complete Mesocolic Excision in Patients With Colon Cancer: Three-year Results From a Prospective, Nonrandomized, Double-blind, Controlled Trial. Ann Surg 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Kim NK, Kim YW, Han YD, et al. Complete mesocolic excision and central vascular ligation for colon cancer: Principle, anatomy, surgical technique, and outcomes. Surg Oncol 2016;25:252-62. [Crossref] [PubMed]
- Negoi I, Beuran M, Hostiuc S, et al. Surgical Anatomy of the Superior Mesenteric Vessels Related to Pancreaticoduodenectomy: a Systematic Review and Meta-Analysis. J Gastrointest Surg 2018;22:802-17. [Crossref] [PubMed]
- Hohenberger W, Weber K, Matzel K, et al. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis 2009;11:354-64; discussion 364-5. [Crossref] [PubMed]
- Gouvas N, Agalianos C, Papaparaskeva K, et al. Surgery along the embryological planes for colon cancer: a systematic review of complete mesocolic excision. Int J Colorectal Dis 2016;31:1577-94. [Crossref] [PubMed]
- West NP, Hohenberger W, Weber K, et al. Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 2010;28:272-8. [Crossref] [PubMed]
- Wang C, Gao Z, Shen K, et al. Safety, quality and effect of complete mesocolic excision vs non-complete mesocolic excision in patients with colon cancer: a systemic review and meta-analysis. Colorectal Dis 2017;19:962-72. [Crossref] [PubMed]
- Alhassan N, Yang M, Wong-Chong N, et al. Comparison between conventional colectomy and complete mesocolic excision for colon cancer: a systematic review and pooled analysis: A review of CME versus conventional colectomies. Surg Endosc 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Agalianos C, Gouvas N, Dervenis C, et al. Is complete mesocolic excision oncologically superior to conventional surgery for colon cancer? A retrospective comparative study. Ann Gastroenterol 2017;30:688-96. [PubMed]
- Bertelsen CA, Neuenschwander AU, Jansen JE, et al. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol 2015;16:161-8. [Crossref] [PubMed]
- Bertelsen CA, Neuenschwander AU, Jansen JE, et al. Short-term outcomes after complete mesocolic excision compared with ‘conventional’ colonic cancer surgery: Complete mesocolic excision versus ‘conventional’ colonic cancer surgery. Br J Surg 2016;103:581-9. [Crossref] [PubMed]
- Merkel S, Weber K, Matzel KE, et al. Prognosis of patients with colonic carcinoma before, during and after implementation of complete mesocolic excision. Br J Surg 2016;103:1220-9. [Crossref] [PubMed]
- Kotake K, Kobayashi H, Asano M, et al. Influence of extent of lymph node dissection on survival for patients with pT2 colon cancer. Int J Colorectal Dis 2015;30:813-20. [Crossref] [PubMed]
- Storli KE, Søndenaa K, Furnes B, et al. Short term results of complete (D3) vs. standard (D2) mesenteric excision in colon cancer shows improved outcome of complete mesenteric excision in patients with TNM stages I-II. Tech Coloproctol 2014;18:557-64. [Crossref] [PubMed]
- An MS, Baik H, Oh SH, et al. Oncological outcomes of complete versus conventional mesocolic excision in laparoscopic right hemicolectomy. ANZ J Surg 2018;88:E698-702. [Crossref] [PubMed]
- Zurleni T, Cassiano A, Gjoni E, et al. Correction to: Surgical and oncological outcomes after complete mesocolic excision in right-sided colon cancer compared with conventional surgery: a retrospective, single-institution study. Int J Colorectal Dis 2018;33:113-4. [Crossref] [PubMed]
- Bernhoff R, Sjövall A, Buchli C, et al. Complete mesocolic excision in right‐sided colon cancer does not increase severe short‐term postoperative adverse events. Colorectal Dis 2018;20:383-389. [Crossref] [PubMed]
- Furnes B, Storli KE, Forsmo HM, et al. Risk Factors for Complications following Introduction of Radical Surgery for Colon Cancer: A Consecutive Patient Series. Scand J Surg 2018. [PubMed]
- Bertelsen CA, Larsen HM, Neuenschwander AU, et al. Long-term Functional Outcome After Right-Sided Complete Mesocolic Excision Compared With Conventional Colon Cancer Surgery: A Population-Based Questionnaire Study. Dis Colon Rectum 2018;61:1063-72. [Crossref] [PubMed]
- Negoi I, Beuran M, Hostiuc S, et al. Surgical Anatomy of the Superior Mesenteric Vessels Related to Colon and Pancreatic Surgery: A Systematic Review and Meta-Analysis. Sci Rep 2018;8:4184. [Crossref] [PubMed]
- Negoi I, Hostiuc S, Negoi RI, et al. Laparoscopic vs open complete mesocolic excision with central vascular ligation for colon cancer: A systematic review and meta-analysis. World J Gastrointest Oncol 2017;9:475-91. [Crossref] [PubMed]
- Olofsson F, Buchwald P, Elmståhl S, et al. No benefit of extended mesenteric resection with central vascular ligation in right-sided colon cancer. Colorectal Dis 2016;18:773-8. [Crossref] [PubMed]
Cite this article as: Negoi I, Beuran M, Hostiuc S, Sartelli M, Coccolini F, Vartic M, Pinkney T. Complete mesocolic excision for colon cancer is technically challenging but the most oncological appealing. Transl Gastroenterol Hepatol 2018;3:79.


