Minimally invasive surgery for gastric gastrointestinal stromal tumors
Introduction
Over the past 2 decades, minimally invasive surgery has emerged as the standard of care for surgical procedures of the appendix, gallbladder, spleen, and colon. Laparoscopic procedures confer perioperative benefits of shortened hospitalization, faster recovery, earlier oral intake as compared to the traditional open procedures (1-6). Similarly, these benefits have been observed when laparoscopic resection is performed for gastric gastrointestinal stromal tumors (GIST). Numerous retrospective case control studies have confirmed the benefits of faster recovery, lower perioperative morbidity and overall superior short-term outcomes of laparoscopic versus open resection for gastric GISTs (7,8). However, studies reporting on long term oncological outcomes of minimally invasive surgery for gastric GIST remains limited (7) and no randomized trials have been reported to date. Nonetheless, level 1 evidence from randomized trials have reported equivalent oncological outcomes of laparoscopic surgery for gastric and colorectal cancers (9,10). Laparoscopic lymphadenectomy and adequate resection margins have also been shown to be technically reproducible and feasible (4-6,9,10). These promising results can be extrapolated to laparoscopic resection of gastric GISTs because of a similar, if not lower, level of complexity of oncological resection. More recently, propensity matched analysis and matched case control studies have been reported similarly supporting the oncological safety for laparoscopic resection for gastric GISTs (11).
The surgical approach for gastric GISTs is usually straightforward in expert hands because local resection is adequate and formal gastrectomy with regional lymphadenectomy is not usually required (12,13). Even though ideally tumor-free resection margins should be obtained, wide resection margins are not mandatory unlike gastric adenocarcinomas as submucosal lymphatic spread does not occur. Furthermore, it has been observed that microscopically involved margins have no apparent detrimental effect on overall survival after complete surgical resection for GIST (14). The favorable disease biology of GIST, allows laparoscopic organ sparing surgery in the majority of cases with excellent long term functional outcomes. In a prospective single institution study, the average Gastrointestinal Quality of Life Index (GIQLI) of the patients who underwent laparoscopic gastric wedge resection was similar to otherwise healthy participants. With the exception of a minority of the patients (~10%) having worse regurgitation symptoms, the majority had a GIQLI within normal range, correlating with an excellent quality of life (15).
Resection for tumors in difficult locations
As shown in many studies, organ sparing surgery in the form of wedge resections can be carried out expeditiously for most gastric GISTs in favorable locations such as the anterior wall and greater curve of the stomach (6-8). However, this approach is sometimes challenging in difficult anatomic locations, such as the gastric cardia or distal antrum. A recent study presented the feasibility of laparoscopic wedge resections for GIST at these difficult locations under the guidance of intraoperative endoscopy. In that study, over 40% of the cases presented were located in the lesser curve, antrum or cardiac. Wedge resection guided by intraoperative endoscopy resulted in a 100% R0 resection with similarly favorable perioperative and long term oncological outcomes, where over 95% 5-year overall survival was achieved (16). More complex approaches such as the intragastric or “endoluminal” surgery through the use of intra-gastric working ports have also been described for challenging locations such as posterior wall gastric GISTs (17,18). Tumors in the abovementioned locations require more advanced laparoscopic skills such as suture manipulation of the tumour, intra-gastric dissection and intra-corporeal suturing to achieve safe resection and reconstruction.
When treating gastric GISTs, the surgeon should be aware of the rare and challenging situation of an extra-intestinal GISTs. These lesions when located posterior to the stomach, have a tendency to invade the surrounding structures such as the pancreas and spleen necessitating a more complex and extensive surgical procedure which might be challenging if attempted laparoscopically (19). The open approach remains the preferred surgical approach for GISTs that require complex multivisceral resection or large lesions that require delicate tissue handling (to prevent tumor rupture) or necessitating a large incision for specimen retrieval (20).
Resection for large GISTs
Despite the advances and increasingly widespread adoption of minimally invasive surgery for gastric GISTs, intraoperative rupture of GISTs remains a significant challenge especially for large cystic GISTs. Should tumor rupture and spillage occur, the prognosis of the patient will be significantly compromised and this should be weighed against the perioperative benefits of the laparoscopic approach (11,21). However, with favorable case selection and expertise in minimally invasive surgery, several authors have reported that selected cases of large gastric GISTs can safely undergo laparoscopic resection (22-24) with minimal risk of rupture. In two recent studies which compared the outcomes of laparoscopic versus open resection of gastric GISTs larger than 5 cm, the laparoscopic approach continued to yield superior perioperative outcomes with no significant differences in complication rates (overall morbidity ~10%, major morbidity <5%, perioperative mortality 1% or less), 5-year disease free survival rates at around 92% or overall survival rates over 93% (24,25). Similarly, results from expert centers have also demonstrated that laparoscopic resection is safe and feasible even for tumors located in unfavorable locations (26).
Comparison between laparoscopic versus open resection for GISTs
To date, several large case-control studies have reported on the outcomes of laparoscopic resection of gastric GIST in comparison with conventional open resection. Tables 1-3 summarizes the results from several of these large (n>50) case-control studies demonstrating that laparoscopic resection can be performed with a low conversion rate and was associated with superior perioperative outcomes such as shorter hospital stay, earlier oral intake, lower morbidity with similar oncological outcomes compared to the open approach (27-32). Similarly, several systematic reviews and meta-analyses have demonstrated that laparoscopic resection was superior in perioperative outcomes compared to open surgery (33-35). In the latest systematic review of 24 studies involving 2,140 patients demonstrated that laparoscopy was associated with superior outcomes including decreased operative time [weighted mean difference (WMD), −30.71 min; 95% CI, −58.48 to −2.95]; decreased intraoperative blood loss (WMD, −60.90 mL; 95% CI, −91.53 to −30.28); decreased time to flatus (WMD, −1.10 days; 95% CI, −1.41 to −0.79); decreased time to oral intake (WMD, −1.25 days; 95% CI, −1.64 to −0.86); decreased length of hospital stay (WMD, −3.42 days; 95% CI, −4.37 to −2.46); decreased morbidity (OR, 0.38; 95% CI, 0.27–0.54); and lower recurrence (OR, 0.45; 95% CI, 0.30–0.66) (35). Nonetheless, it is important to emphasize that current evidence in support of the minimally invasive approach is presently limited to retrospective case control studies with an inherent potential for selection bias. However, although ideal, the rarity of GIST and the lack of obvious therapeutic equipoise makes prospect of conducting a prospective randomized control trial difficult today.
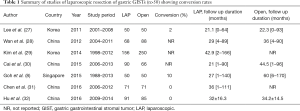
Full table

Full table
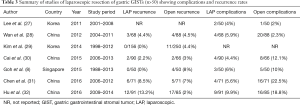
Full table
Robotic resection for GISTs
Robotic surgery was first introduced to overcome the limitations of conventional laparoscopy especially with the high definition 3D monitor and the increased dexterity of the robotic arms. With regards to resection for gastric GISTs, the robotic approach potentially expands the indications of minimally invasive surgery by enabling minimally invasive procedures for tumors located in places that are more difficult to access via conventional laparoscopic surgery such as in the cardioesophageal and duodenogastric junctions. It also simplifies complex tasks such as intracorporeal suturing in difficult locations (36). Presently, experience with robotic resection for gastric GISTs remains limited. However, several small case series have demonstrated the oncological safety, low complication and low conversion rates associated with robotic assisted excision of large GISTs (>5 cm) in difficult locations (37-41). However, robotic assistance has been reported to be associated with an increase in operating time and its cost-effectiveness remain a major obstacle to the widespread adoption of this technology.
Conclusions
In summary, minimally surgery for gastric GISTs has been widely adopted today and is an excellent procedure especially for tumors in favorable locations within the stomach allowing patients to enjoy superior perioperative outcomes over the open approach without compromising oncological outcomes. In expert hands, the surgical indications can potentially be safely expanded to large tumors or tumors in difficult locations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Keus F, de Jong JA, Gooszen HG, et al. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev 2006.CD006231. [PubMed]
- Barbaros U, Dinççağ A, Sümer A, et al. Prospective randomized comparison of clinical results between hand-assisted laparoscopic and open splenectomies. Surg Endosc 2010;24:25-32. [Crossref] [PubMed]
- Mehrabi A, Hafezi M, Arvin J, et al. A systematic review and meta-analysis of laparoscopic versus open distal pancreatectomy for benign and malignant lesions of the pancreas: it's time to randomize. Surgery 2015;157:45-55. [Crossref] [PubMed]
- van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210-8. [Crossref] [PubMed]
- Kim W, Kim HH, Han SU, et al. Decreased Morbidity of Laparoscopic Distal Gastrectomy Compared With Open Distal Gastrectomy for Stage I Gastric Cancer: Short-term Outcomes From a Multicenter Randomized Controlled Trial (KLASS-01). Ann Surg 2016;263:28-35. [Crossref] [PubMed]
- Koh YX, Chok AY, Zheng HL, et al. A systematic review and meta-analysis comparing laparoscopic versus open gastric resections for gastrointestinal stromal tumors of the stomach. Ann Surg Oncol 2013;20:3549-60. [Crossref] [PubMed]
- Bischof DA, Kim Y, Dodson R, et al. Open versus minimally invasive resection of gastric GIST: a multi-institutional analysis of short- and long-term outcomes. Ann Surg Oncol 2014;21:2941-8. [Crossref] [PubMed]
- Goh BK, Goh YC, Eng AK, et al. Outcome after laparoscopic versus open wedge resection for suspected gastric gastrointestinal stromal tumors: A matched-pair case-control study. Eur J Surg Oncol 2015;41:905-10. [Crossref] [PubMed]
- Boutros M, Hippalgaonkar N, Silva E, et al. Laparoscopic resection of rectal cancer results in higher lymph node yield and better short-term outcomes than open surgery: a large single-center comparative study. Dis Colon Rectum 2013;56:679-88. [Crossref] [PubMed]
- Lu W, Gao J, Yang J, et al. Long-term clinical outcomes of laparoscopy-assisted distal gastrectomy versus open distal gastrectomy for early gastric cancer: A comprehensive systematic review and meta-analysis of randomized control trials. Medicine (Baltimore) 2016;95:e3986. [Crossref] [PubMed]
- Xu C, Chen T, Hu Y, et al. Retrospective study of laparoscopic versus open gastric resection for gastric gastrointestinal stromal tumors based on the propensity score matching method. Surg Endosc 2017;31:374-81. [Crossref] [PubMed]
- DeMatteo RP, Lewis JJ, Leung D, et al. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 2000;231:51-8. [Crossref] [PubMed]
- Chok AY, Koh YX, Ow MY, et al. A systematic review and meta-analysis comparing pancreaticoduodenectomy versus limited resection for duodenal gastrointestinal stromal tumors. Ann Surg Oncol 2014;21:3429-38. [Crossref] [PubMed]
- McCarter MD, Antonescu CR, Ballman KV, et al. Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg 2012;215:53-9. [Crossref] [PubMed]
- Dressler JA, Palazzo F, Berger AC, et al. Long-term functional outcomes of laparoscopic resection for gastric gastrointestinal stromal tumors. Surg Endosc 2016;30:1592-8. [Crossref] [PubMed]
- Mueller CL, Braun J, Leimanis ML, et al. Application of an individualized operative strategy for wedge resection of gastric gastrointestinal stromal tumors: Effectiveness for tumors in difficult locations. Surgery 2016;160:1038-48. [Crossref] [PubMed]
- Novitsky YW, Kercher KW, Sing RF, et al. Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Ann Surg 2006;243:738-45; discussion 745-7. [Crossref] [PubMed]
- Maker AV. A technique for laparoendoscopic resection of posterior fundic gastric GISTs without need for a gastrotomy. Ann Surg Oncol 2013;20:4238. [Crossref] [PubMed]
- Goh BK, Chow PK, Kesavan SM, et al. A single-institution experience with eight CD117-positive primary extragastrointestinal stromal tumors: critical appraisal and a comparison with their gastrointestinal counterparts. J Gastrointest Surg 2009;13:1094-8. [Crossref] [PubMed]
- Casali PG, Jost L, Reichardt P, et al. Gastrointestinal stromal tumours: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol 2009;20 Suppl 4:64-7. [PubMed]
- Demetri GD, von Mehren M, Antonescu CR, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 2010;8 Suppl 2:S1-41. [Crossref] [PubMed]
- Masoni L, Gentili I, Maglio R, et al. Laparoscopic resection of large gastric GISTs: feasibility and long-term results. Surg Endosc 2014;28:2905-10. [Crossref] [PubMed]
- Lin J, Huang C, Zheng C, et al. Laparoscopic versus open gastric resection for larger than 5 cm primary gastric gastrointestinal stromal tumors (GIST): a size-matched comparison. Surg Endosc 2014;28:2577-83. [Crossref] [PubMed]
- Khoo CY, Goh BKP, Eng AK, et al. Laparoscopic wedge resection for suspected large (≥5 cm) gastric gastrointestinal stromal tumors. Surg Endosc 2017;31:2271-9. [Crossref] [PubMed]
- Piessen G, Lefèvre JH, Cabau M, et al. Laparoscopic Versus Open Surgery for Gastric Gastrointestinal Stromal Tumors: What Is the Impact on Postoperative Outcome and Oncologic Results? Ann Surg 2015;262:831-9. [Crossref] [PubMed]
- Huang CM, Chen QF, Lin JX, et al. Can laparoscopic surgery be applied in gastric gastrointestinal stromal tumors located in unfavorable sites?: A study based on the NCCN guidelines. Medicine (Baltimore) 2017;96:e6535. [Crossref] [PubMed]
- Lee HH, Hur H, Jung H, et al. Laparoscopic wedge resection for gastric submucosal tumors: a size-location matched case-control study. J Am Coll Surg 2011;212:195-9. [Crossref] [PubMed]
- Wan P, Yan C, Li C, et al. Choices of surgical approaches for gastrointestinal stromal tumors of the stomach: laparoscopic versus open resection. Dig Surg 2012;29:243-50. [Crossref] [PubMed]
- Kim IH, Kim IH, Kwak SG, et al. Gastrointestinal stromal tumors (GISTs) of the stomach: a multicenter, retrospective study of curatively resected gastric GISTs. Ann Surg Treat Res 2014;87:298-303. [Crossref] [PubMed]
- Cai JQ, Chen K, Mou YP, et al. Laparoscopic versus open wedge resection for gastrointestinal stromal tumors of the stomach: a single-center 8-year retrospective cohort study of 156 patients with long-term follow-up. BMC Surg 2015;15:58. [Crossref] [PubMed]
- Chen QF, Huang CM, Lin M, et al. Short- and long-term outcomes of laparoscopic versus open resection for gastric gastrointestinal stromal tumors: a propensity score-matching analysis. Medicine 2016;95:e3135. [Crossref] [PubMed]
- Hu J, Or BH, Hu K, et al. Comparison of the post-operative outcomes and survival of laparoscopic versus open resections for gastric gastrointestinal stromal tumors: a multi-center prospective cohort study. Int J Surg 2016;33 Pt A:65-71.
- Liang JW, Zheng ZC, Zhang JJ, et al. Laparoscopic versus open gastric resections for gastric gastrointestinal stromal tumors: a meta-analysis. Surg Laparosc Endosc Percutan Tech 2013;23:378-87. [Crossref] [PubMed]
- Zheng L, Ding W, Zhou D, et al. Laparoscopic versus open resection for gastric gastrointestinal stromal tumors: a meta-analysis. Am Surg 2014;80:48-56. [PubMed]
- Xiong H, Wang J, Jia Y, et al. Laparoscopic surgery versus open resection in patients with gastrointestinal stromal tumors: An updated systematic review and meta-analysis. Am J Surg 2017;214:538-46. [Crossref] [PubMed]
- Buchs NC, Bucher P, Pugin F, et al. Robot-assisted oncologic resection for large gastric gastrointestinal stromal tumor: a preliminary case series. J Laparoendosc Adv Surg Tech A 2010;20:411-5. [Crossref] [PubMed]
- Noshiro H, Nomura A, Akashi M, et al. Pure Robotic Surgery for Intraluminally Growing Gastrointestinal Stromal Tumors around the Esophagogastric junction or Pyloric Ring. Hepatogastroenterology 2015;62:629-34. [PubMed]
- de'Angelis N, Genova P, Amiot A, et al. Robotic Versus Laparoscopic Gastric Resection for Primary Gastrointestinal Stromal Tumors >5 cm: A Size-Matched and Location-Matched Comparison. Surg Laparosc Endosc Percutan Tech 2017;27:65-71. [PubMed]
- Desiderio J, Trastulli S, Cirocchi R, et al. Robotic gastric resection of large gastrointestinal stromal tumors. Int J Surg 2013;11:191-6. [Crossref] [PubMed]
- Moriyama H, Ishikawa N, Kawaguchi M, et al. Robot-assisted laparoscopic resection for gastric gastrointestinal stromal tumor. Surg Laparosc Endosc Percutan Tech 2012;22:e155-6. [Crossref] [PubMed]
- Vicente E, Quijano Y, Ielpo B, et al. Robot-assisted resection of gastrointestinal stromal tumors (GIST): a single center case series and literature review. Int J Med Robot 2016;12:718-23. [Crossref] [PubMed]
Cite this article as: Koh YX, Goh BK. Minimally invasive surgery for gastric gastrointestinal stromal tumors. Transl Gastroenterol Hepatol 2017;2:108.


