Feasibility and safety of modified inverted T-shaped method using linear stapler with movable cartridge fork for esophagojejunostomy following laparoscopic total gastrectomy
Introduction
The indications for minimally invasive surgery continue to expand. In fact, endoscopic surgery is currently regarded as standard treatment for patients with numerous conditions. Advances in endoscopic surgery have provided patients with less postoperative pain, shorter hospital stays, and an earlier return to work. With such advances, the performance of laparoscopic distal gastrectomy for patients with early gastric cancer is rapidly becoming more common worldwide (1). However, the performance of laparoscopic total gastrectomy (LTG) is limited because there were the technical difficulties in lymph node dissection and esophagojejunostomy under laparoscopy. The dissection of lymph node station no. 11p, which is defined as D1+ dissection in total gastrectomy, is recommended by the Japanese Gastric Cancer Association (2). Kanaya et al. (3) and Fukunaga et al. (4) reported the medial approach and left-sided approach, respectively, for laparoscopic suprapancreatic lymph node dissection including lymph node station no. 11p. These approaches improved the accuracy, safety, and reproducibility of dissection of lymph node station no. 11p and now are spreading in Japan. Conversely, the use of a circular or linear stapling device has been reported for intracorporeal esophagojejunostomy (5,6). However, techniques using such devices are still associated with several problems. When using a circular stapler, intracorporeal purse-string suturing is difficult, and the OrVil device (Covidien, Mansfield, MA, USA) is associated with a risk of esophageal injury. Additionally, the overlap method reportedly has satisfactory outcomes as a linear stapler technique for intracorporeal esophagojejunostomy (7,8). However, hand sewing to close the common entry hole after stapling remains difficult. Functional end-to-end esophagojejunostomy with a linear stapler can reportedly be performed to avoid this problem (9). However, the use of this method is limited in patients with a sufficiently preserved abdominal esophagus.
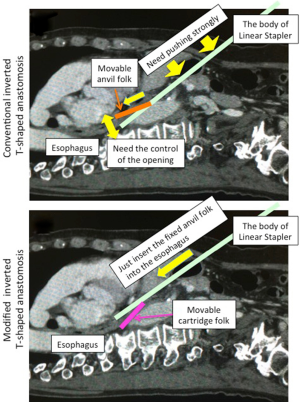
We previously reported use of a modified overlap method to decrease the difficulty associated with hand sewing of the entry hole of the linear stapler (10). In this previous modified method, we divided the esophagus in the ventrodorsal direction and inserted the linear stapler from the anterior wall of the jejunum to the posterior wall. After stapling, the common entry hole is opened upward, which provides a suitable view for hand sewing to close it easily. We used this conventional modified method and performed esophagojejunostomy after LTG without any intraoperative troubles for 61 patients until July 2011. During that period, we used a linear stapler with a fixed cartridge fork. We inserted the fixed cartridge fork to the jejunum to avoid perforation of its posterior wall by the fine movable anvil fork. However, to insert the movable anvil fork to the esophagus using this procedure, we often had to strongly push down the main body of the stapler with the fixed cartridge fork to the dorsal side to bring the direction of the anvil fork in line with the direction of the long axis of the esophagus (Figure 1A). At the same time, we must control the opening of the movable anvil fork (Figure 1A). This procedure is sometimes difficult for surgeons without adequate experience, and a two-handed operation is often needed for manipulation of the linear stapler. To avoid this difficulty, we began using a linear stapler with a movable cartridge fork to perform the inverted T-shaped method in August 2011. In this modified inverted T-shaped method, we inserted the movable cartridge fork into the Roux limb and then inserted the fixed anvil fork into the esophagus. The opening of the movable cartridge fork is naturally and properly controlled when the fixed anvil fork is inserted into the esophagus (Figure 1B). Therefore, surgeons can easily bring the direction of the fixed anvil fork in line with the direction of the long axis of the esophagus using one hand. They do not have to push the main body of the stapler to the dorsal side and control the opening of the movable cartridge fork. Here, we investigated the short-term outcomes of LTG using the modified inverted T-shaped method (movable cartridge fork) and compared them with those of the conventional method (fixed cartridge fork).
Methods
Patients
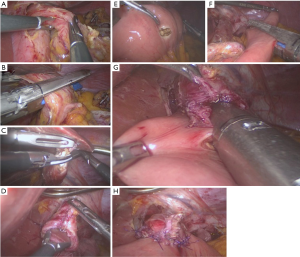
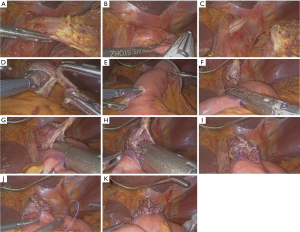
We performed LTG in a total of 155 consecutive patients with gastric cancer from November 2007 to December 2015 in Kyushu University Hospital. After LTG, we performed the conventional inverted T-shaped method using a linear stapler with a fixed cartridge fork (Figure 2) in 61 patients from November 2007 to July 2011 (fixed cartridge group). From August 2011, we used a linear stapler with a movable cartridge fork and performed the modified inverted T-shaped method (Figure 3) in 94 patients (movable cartridge group).
Surgical procedures
We performed LTG procedure as previously described (10). The esophagus was rotated and divided in the ventrodorsal direction (Figures 2A,B,3A,B,C). We then resected the jejunum 30 cm from the duodenojejunal junction, prepared 40-cm Roux limb through the antecolic route and performed Roux-en-Y reconstruction. We performed esophagojejunal anastomosis with either a 45-mm fixed blue-cartridge (fixed cartridge group) or a 45-mm movable purple-cartridge (movable cartridge group). First, we made small incisions at the dorsal edge of the esophageal stump (Figures 2C,D,3D) and the anterior wall of the jejunum 50 mm from the stump of the Roux limb (Figures 2E,3E). The 45-mm fixed blue-cartridge (fixed cartridge group) or the 45-mm movable purple-cartridge (movable cartridge group) was then inserted through the small incision in the anterior wall of the Roux limb. We placed the staple line in the direction of the posterior wall of the Roux limb (Figures 2F,3F), and then lifted up the linear stapler to the anastomotic site to ensure that the mesenteric tension was low. Sufficient lower esophageal exposure was also ensured to avoid the perforation of the jejunum by the jaw of the linear stapler during firing. At last, we inserted the movable or fixed anvil fork into the small incision in the stump of esophagus (Figures 2G,3G,H). After the anastomosis with the linear stapler (Figure 3I), we closed the common entry hole by hand sewing (Figures 2H,3J,K).
Statistics
We obtained the patients’ clinical data from their medical records and performed statistical analysis using the Wilcoxon rank sum test for continuous variables and the unpaired chi-square test for categorized variables. We expressed all values as mean ± standard deviation. A P value of <0.05 was considered significant. We used the JMP 8.0 program (SAS Institute, Cary, NC, USA) for the present statistical analyses.
Results
Patient characteristics
As shown in Table I, the patients in the movable and fixed cartridge groups were characterized. The mean age and male-to-female ratio in the movable cartridge group were comparable with those in the fixed cartridge group. We found no difference in the ratio of advanced to early carcinoma between the movable and fixed cartridge groups. According to the Japanese Classification of Gastric Carcinoma, 2nd English Edition (11), we determined the clinical stages and found no significant differences in the clinical depth of invasion or cancer stages between the movable and fixed cartridge groups. However, there was a significant difference in the clinical nodal involvement between the movable and fixed cartridge groups. Patients in the movable cartridge group had higher N stages than did those in the fixed cartridge group (P=0.0109).
Perioperative information
As shown in Table II, we found no significant differences in the operative time or blood loss between the movable and fixed cartridge groups. Open conversion was not encountered in this series. In the fixed cartridge group, 17 of 61 patients underwent LTG combined with splenectomy and 1 patient underwent LTG combined with splenectomy and pancreatic tail resection. In the movable cartridge group, three patients underwent combined resection of the spleen, pancreatic tail with the spleen, and transverse colon, respectively. We performed laparoscopic cholecystectomy in 11 patients in the movable cartridge group and 7 patients in the fixed cartridge group. As synchronous operations, two laparoscopic colectomies and one laparoscopic nephrectomy were performed in the movable cartridge group, and one laparoscopic colectomy and one laparoscopic nephrectomy were performed in the fixed cartridge group. We found no differences in number of harvested or metastatic lymph nodes between the movable and fixed cartridge groups.
Postoperative findings
As shown in Table III, we summarized the postoperative course. The fixed cartridge group included seven patients with intra-abdominal morbidities: one anastomotic leakage (1.6%), one anastomotic stenosis (1.6%), one abdominal bleed (1.6%), two pancreatic leakages (3.3%), and two duodenal stump leakages. There were four intra-abdominal morbidities in the movable cartridge group: one anastomotic stenosis (1.1%), one anastomotic bleed (1.1%), one pancreatic leakage (1.1%), and one abdominal abscess (1.1%). We found no significant difference in the postoperative hospital stay between the movable and fixed cartridge groups (13.0±14.7 vs. 14.6±12.5 days, respectively). According to the pathological reports, we found no significant difference in the pathological depth of invasion or pathological nodal involvement between the movable and fixed cartridge groups.
Discussion
Laparoscopic surgery has been widely performed for gastric cancer. However, surgeons are generally less familiar with LTG than laparoscopic distal gastrectomy partly because of the difficulty of intra-abdominal esophagojejunostomy. Two major devices are used for esophagojejunostomy after total gastrectomy in both open and laparoscopic surgery: the circular stapler and the linear stapler. Many reports to date have described both the circular stapling method and linear stapling method, and selection of the stapling method for esophagojejunostomy after LTG is usually dependent upon the surgeon’s preference.
We also previously reported the feasibility and safety of our novel modified overlap method using a linear stapler (Figure 2), termed inverted T-shaped anastomosis (10). Until July 2011, we successfully performed the inverted T-shaped method using a linear stapler with a fixed cartridge fork in 61 cases. However, we encountered some technical problems when the movable anvil fork of the stapler was inserted into the esophagus. In the conventional inverted T-shaped method, the fixed cartridge fork of the stapler was then inserted into the lumen of the Roux limb from the small incision in the anterior wall toward the posterior wall, and the movable anvil fork was inserted into the esophagus (Figure 2G). Therefore, after stapling for esophagojejunostomy, a good operative view is provided to close the common entry hole by hand sewing because its hole opened upward. In these procedures, we inserted the fixed cartridge fork into the lumen of the Roux limb to avoid the perforation of the jejunum by the jaw of the linear stapler because the tip of the fixed cartridge fork was duller than that of the movable anvil fork. However, surgeons without sufficient experience encountered some technical difficulties when the movable anvil fork was inserted into the esophagus. The surgeon must bring the direction of the movable anvil fork in line with the direction of the long axis of the esophagus in the open-jaw state when they insert the movable anvil fork into the esophagus. To do this, the surgeon must strongly push down the body of the stapler with the fixed cartridge fork to the dorsal side while simultaneously controlling the opening of the jaw (Figures 1A,2G). Therefore, for surgeons without sufficient experience, two hands are sometimes needed to operate the stapler.
To resolve this problem and facilitate safer performance of the esophagojejunostomy, we modified the inverted T-shaped method using the linear stapler with the removable cartridge fork beginning in August 2011. To date, we have successfully performed the modified inverted T-shaped method in 94 patients. In this modified procedure, we use a linear stapler with a movable cartridge fork and insert it into the Roux limb (Figure 3G,H). We then easily insert the fixed anvil fork into the esophagus without the need to push down the body of the linear stapler and control the opening of the jaw of stapler because the opening of the movable cartridge fork is naturally and properly controlled when the fixed anvil fork is inserted into the esophagus (Figure 1B).
In the present study, we found no significant differences in the perioperative or postoperative events between the movable and fixed cartridge groups. One case of anastomotic leakage occurred in the fixed cartridge group, but no anastomotic leakage occurred in the movable cartridge group. The effects of learning and technical advancements with the surgeons’ increasing experience may have affected the results. Although further long-term follow-up will be needed, to confirm the reliability and the feasibility of this modified method, the opening of the movable cartridge fork is naturally and properly controlled when the fixed anvil fork is inserted into the esophagus. Therefore, surgeons can easily bring the direction of the fixed anvil fork in line with the direction of the long axis of the esophagus using one hand. We believe that the modified inverted T-shaped method is more feasible and reliable than the conventional method and will contribute to the improved safety of LTG.
Acknowledgements
Funding: This work was supported in part by a Japan Society for the Promotion of Science Grant-in-Aid for Scientific Research (B) and (C) and Scientific Research on Innovative Areas (Grant No. 26293305).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical statement: Written informed consent was obtained from the all patients for use of their data in the clinical research although we used only unlinkable anonymized data in the present study.
References
- Bamboat ZM, Strong VE. Minimally invasive surgery for gastric cancer. J Surg Oncol 2013;107:271-6. [Crossref] [PubMed]
- Sano T, Sasako M, Yamamoto S, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol 2004;22:2767-73. [Crossref] [PubMed]
- Kanaya S, Haruta S, Kawamura Y, et al. Video: laparoscopy distinctive technique for suprapancreatic lymph node dissection: medial approach for laparoscopic gastric cancer surgery. Surg Endosc 2011;25:3928-9. [Crossref] [PubMed]
- Fukunaga T, Hiki N, Tokunaga M, et al. Left-sided approach for suprapancreatic lymph node dissection in laparoscopy-assisted distal gastrectomy without duodenal transection. Gastric Cancer 2009;12:106-12. [Crossref] [PubMed]
- Jeong O, Park YK. Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc 2009;23:2624-30. [Crossref] [PubMed]
- Walther BS, Zilling T, Johnsson F, et al. Total gastrectomy and oesophagojejunostomy with linear stapling devices. Br J Surg 1989;76:909-12. [Crossref] [PubMed]
- Uyama I, Sugioka A, Matsui H, et al. Laparoscopic side-to-side esophagogastrostomy using a linear stapler after proximal gastrectomy. Gastric Cancer 2001;4:98-102. [Crossref] [PubMed]
- Inaba K, Satoh S, Ishida Y, et al. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 2010;211:e25-9. [Crossref] [PubMed]
- Ebihara Y, Okushiba S, Kawarada Y, et al. Outcome of functional end-to-end esophagojejunostomy in totally laparoscopic total gastrectomy. Langenbecks Arch Surg 2013;398:475-9. [Crossref] [PubMed]
- Nagai E, Ohuchida K, Nakata K, et al. Feasibility and safety of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy: inverted T-shaped anastomosis using linear staplers. Surgery 2013;153:732-8. [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma - 2nd English Edition -. Gastric Cancer 1998;1:10-24. [Crossref] [PubMed]
Cite this article as: Ohuchida K, Nagai E, Moriyama T, Shindo K, Manabe T, Ohtsuka T, Shimizu S, Nakamura M. Feasibility and safety of modified inverted T-shaped method using linear stapler with movable cartridge fork for esophagojejunostomy following laparoscopic total gastrectomy. Transl Gastroenterol Hepatol 2017;2:50.


