Is partial omentectomy feasible at radical gastrectomy for advanced cancer?
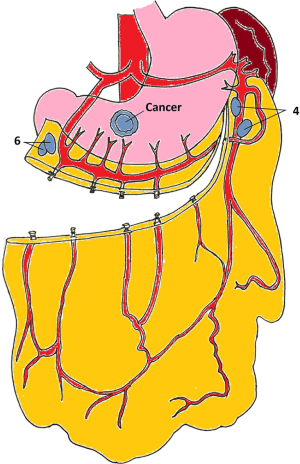
We read with interest the article “Role of omentectomy as part of radical surgery for gastric cancer” published by Jongerius et al. in the British Journal of Surgery (1). In that study, 100 total omentectomy specimens, all procured during gastric cancer surgeries, were examined histopathologically. Authors allocated the omentectomy specimens from the stomach along the distal margin of the gastroepiploic (GE) arcus. When these omentectomy specimen were examined histopathologically, the researchers found malignancies in five omentum samples that was a marker of an advanced disease. They concluded that the total removal of omentum was thought to have limited benefit to systemic disease. For this reason, routine application of total omentectomy was not suggested. We found the results of this study, which questioned the role of omentectomy during radical gastrectomy, encouraging and rational. However, in this study, the omentum was separated from the distal from the GE arcus. In order to supply the remaining omentum, either the right GE artery or the left GE artery needs to be intact (Figure 1) (2). In an advanced gastric cancer located in the distal region, it may be necessary to remove the right GE artery in order to receive 6-no lymph nodes and to close the duodenal stump. The left GE artery should then be protected. For the preservation of the left GE artery, the stomach-omentum separation must be done very close to the stomach (Figure 1). In this case, there is a risk that the 4-no lymph nodes along the large curvature cannot be removed (Figure 1). The same problem is more pronounced for 1/3 mid or 1/3 proximal tumors. Preservation requirement of one of the GE arcs for partial omentectomy and the appropriate lymph node dissection are the two sides of the problem. Preservation of distal omentum in gastric cancer surgery may not cause an oncological disadvantage. However, close-to-stomach omental separation may prevent the removal of certain lymph nodes along the large curvature, so that the remaining omentum can prevented from ischemia. The number of studies involving partial omentectomy in the surgery of gastric cancer was limited and these were usually done for early gastric cancer (3). Partial omentectomy should be further discussed in advanced cancers. It should be keep in mind that remnant omental ischemia can also be seen in patients with partial omentectomy (4).
Omentum majus forms the inferion-anterior wall of bursa omentalis. Total omentectomy has been recommended for the completion of bursectomy in gastric cancer surgery; however, the role of bursectomy in gastric cancer surgery is also a debate (5). As a result, oncologically, leaving a portion of the omentum under the GE arcs back may not be a problem. However, technically, it is still unclear how to achieve it, without causing omental ischemia and allowing the collecting of lymph nodes along the GE arcus. It is clear that more trials need to be done both in terms of oncologic outcomes and omental ischemia.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jongerius EJ, Boerma D, Seldenrijk KA, et al. Role of omentectomy as part of radical surgery for gastric cancer. Br J Surg 2016;103:1497-503. [Crossref] [PubMed]
- Meffert-Liebermann D. Greater Omentum: Anatomy, Physiology, Pathology, and Surgery With a Historical Survey. 1st Edition. Springer-Verlag, 1983.
- Kim MC, Kim KH, Jung GJ, et al. Comparative study of complete and partial omentectomy in radical subtotal gastrectomy for early gastric cancer. Yonsei Med J 2011;52:961-6. [Crossref] [PubMed]
- Oh JY, Cho JH, Kang MJ, et al. Omental infarction caused by laparoscopy-assisted gastrectomy for gastric cancer: CT findings. Clin Radiol 2011;66:966-73. [Crossref] [PubMed]
- Kayaalp C. Bursectomy at radical gastrectomy. World J Gastrointest Surg 2015;7:249-53. [Crossref] [PubMed]
Cite this article as: Aktas A, Gundogan E, Sumer F, Kayaalp C. Is partial omentectomy feasible at radical gastrectomy for advanced cancer? Transl Gastroenterol Hepatol 2017;2:13.


