Primary hepatic neuroendocrine tumor: report of one case
Case presentation
History
A 41-year-old female patient was admitted due to “a hepatic mass found 2 weeks ago”. In this patient, right breast cancer was confirmed 2 weeks ago. Meanwhile, abdominal CT indicated the presence of an irregular mass sized 8.9 cm × 6.3 cm in the right lobe of liver. The lesion was considered to be malignant; however, whether it was a primary or metastatic lesion required further clarification. Liver MRI was suggestive of an adenoma, and the possibility of a malignant change could not be ruled out. The patient underwent simple resection of right breast + sentinel lymph node biopsy in right breast, and ductal carcinoma in situ (DCIS) was pathologically confirmed in right breast. The patient had no discomfort and further received the resection of liver tumor.
She had been hypertensive for 3 years. The blood pressure was maintained at 130/80 mmHg by oral administration of antihypertensives. She was allergic to penicillin. Her marriage and childbearing history, personal history, and family history had no special records.
Diagnosis and treatment
Physical examination
The vital signs were stable. No superficial lymph node was palpable throughout the body. The right breast was absent. Heart and lung showed no obvious abnormality. The abdomen was flat and soft, without any tenderness or rebound tenderness. Liver and spleen were not palpable under ribs. Bowel sounds were normal. No swelling of lower limbs was observed.
Auxiliary examination
Routine blood tests, blood biochemistry, blood coagulation test, viral tests, and tumor marker determinations showed no significant abnormality.
Abdominal MRI: (I) a mass sized 11.2 cm × 7.7 cm was found in the right lobe of liver. It showed slightly low signal on T1WI and unevenly high signal on T2WI/FS. Restricted diffusion was obvious on DWI. After contrast agent administration, the lesion was obviously enhanced during the early phase. While the enhancement was decreased during the delayed phase, patchy enhancement zones could still be seen inside the lesion. An adenoma was considered, and the possibility of a malignant change could not be ruled out; (II) spotty enhancement was seen within the left hepatic lobe. It showed equal signal during the portal venous phase and during plain scans. The possibility of abnormal blood supply was considered (Figure 1).
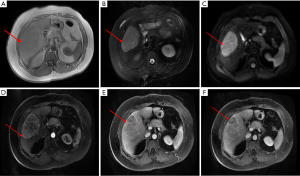
A mass in the right lobe of liver.
Diagnosis:
- A space-occupying lesion in liver. An adenoma? Liver cancer?
- Hypertension.
Treatment
Irregular hepatectomy was performed in the right liver on December 2, 2014.
Postoperative pathology and immunohistochemistry
Right liver and the tumor: a neuroendocrine tumor (NET); G2; mitotic figures: 4/10 HPF; no definite vascular thrombosis or nerve infiltration was observed.
Immunohistochemical findings included: AFP(−), hepatocyte(−), CD34 (hepatic sinusoid capillatization), CK7(−), CK18(3+), Ki-67(+10%), ER(−), PR (lesion was weakly positive), GCDFP-15(−), CDX2(1+), CK20(−), syn(2+), CgA(1+), CD56(−), CEA(−), and CK19(3+).
Postoperative supplementary examinations
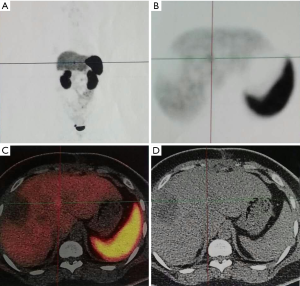
Somatostatin receptor (SSRT) scintigraphy (on December 18, 2014): the SSTR was not highly expressed in the lesion.
18F-FDG PET/CT (on December 17, 2014): the images showed focal increased uptake of 18F-FDG in the right side of the sternum, with unknown nature. The uptake of 18F-FDG in systemic bone marrow was unevenly increased, with unknown nature.
68Ga-DOTA-TATE ET/CT (on January 7, 2015): a hepatic lesion with increased uptake of the agent was seen (sized 1.1 cm × 1.9 cm, with SUVmax 10.0) (Figure 2).
Discussion
Features of hepatic NETs
Traditionally it was believed that the primary hepatic neuroendocrine tumor (PHNET) arose from ectopic pancreatic tissues or from intrahepatic adrenal tissues. However, research has shown that PHNET is more likely to be caused by the proliferation of neuroendocrine cells in intrahepatic bile duct. PHNET is an extremely rare disease. In China, only 47 PHNET cases were reported between 1994 and 2010. The patients aged 15–84 years (mean: 51 years), with a male/female ratio of 0.96 (23/24), which was consistent with the data reported in foreign countries. Missed diagnosis or misdiagnosis is common for PHNET due to its low prevalence and non-specific clinical symptoms. Furthermore, it is a highly malignant change and can be associated with liver metastasis or regional lymph node metastasis in its early stage. Thus, the prognosis is often poor. Early diagnosis and timely treatment may help to prolong the survival of PHNET patients.
Diagnostic methods of hepatic NETs
While NETs are most commonly seen in the gastrointestinal tract (accounting for 67.5%), PHNETs account for only 0.34%. However, liver is the most commonly site for metastatic disease from gastrointestinal NETs. Therefore, the possible primary lesion should be explored for any clinically identified hepatic NETs. A diagnosis of primary NETs should not be made before the possibility of a metastatic lesion is ruled out.
The diagnosis of hepatic NETs relies mainly on pathology and Immunohistochemistry. In addition, medical imaging approaches are also helpful for the preoperative diagnosis of hepatic NETs; however, their findings are not specific. The possible imaging findings may include: (I) size and morphology: hepatic NETs are generally large (>5 cm in diameter), with round or irregular shape and clear margin. The tumor can be either solitary or multiple. The multiple tumor is often featured by a large tumor surrounded by many small tumors, which is a characteristic presentation of PHNETs; (II) plain scans: the lesion often shows low density on plain CT scans. During MRI plain scans, it shows low signal on T1WI and slightly high signal on T2WI. When the tumor becomes larger, its center often develops obsolete bleeding, necrosis, and cystic changes, which are shown as big or small lower-density areas on CT. During MRI, the lesion shows even lower signal on T1WI and higher signal on T2WI. Moreover, T2WI might better reflect the pathological features of this tumor. Tumor calcification may be seen in a few cases; (III) contrast-enhanced scans: mild or moderate enhancement may be seen in the tumor entity; however, the degree of enhancement is not as high as NETs in the susceptible sites (e.g., the pancreas). The enhancement patterns may be as follows: (I) enhancement in the early phase, followed by the decreased enhancement in later phases; (II) without obvious enhancement in the early phase, followed by slight enhancement in later phases, with the densities or signals lower than the surrounding normal liver parenchyma; (III) secondary manifestations: even when the tumor becomes very large, it seldom invades vessels nearby.
Treatment of hepatic NETs
Similar to NETs in other sites, PHNET is mainly treated by surgery. However, the prognosis of NETs can be highly diverse due to the difference in differentiation degree. Chemotherapy can achieve a response rate of 40–70% in patients with unresectable gastrointestinal NETs, thus its role cannot be neglected. Since the tumors arise from the same tissues, chemotherapy theoretically can achieve similar efficacies in the treatment of PHNECs; however, the exact efficacies require further investigation. Positive SSTR expression was found in about 55–95% of GEP-NETs cell surface, which can be in combination with the specificity of somatostatin analogs (SSTA) (e.g., octreotide). SSTA has shown good efficacy for functional SSTR-positive NETs; however, its role in treating non-functional NETs remains unclear. SSTA treatment may be considered for functional PHNEC; however, currently no relevant report has been available.
Summary
PHNEC is an extremely rare tumor. Since its clinical manifestations are not specific, immunohistochemistry has a particularly important role in diagnosing PHNEC. Meanwhile, the possibility of metastatic NEC should be ruled out first. While few literatures have described the treatment and prognosis of PHNEC, surgical resection remains the mainstream treatment. The treatment strategies for GEP-NETs may be valuable.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Cite this article as: Hu X, Huang Z, Zhang Y, Chen X, Zhao H, Bi X. Primary hepatic neuroendocrine tumor: report of one case. Transl Gastroenterol Hepatol 2016;1:82.


