Pancreatic neuroendocrine cancer with liver metastases and multiple peritoneal metastases: report of one case
Disease history and treatment
A 59-year-old male patient was found to be with an abdominal wall neoplasm in April 2012. No special treatment was applied. Since then he suffered from passage of loose stools (4–5 times daily), and the stool volume was relatively large. His body weight decreased by 5 kg, although he had no facial flushing, bronchial spasm, faint, blood glucose fluctuations, or erythema migrans. He had no other history of disease.
Computed tomography (CT) performed in other hospital revealed the presence of a mass at the head of pancreas. Multiple liver metastases as well as multiple masses in greater omentum, mesentery, and abdominal and pelvic cavities were observed and considered to be metastatic lesions.
Liver biopsy in other hospital revealed the presence of adenocarcinoma invasion within the fibrous tissue. A diagnosis of tumor could not be confirmed during a pathological consultation in our hospital.
Tumor markers: AFP, CEA, CA125, CA199, and CA153 were normal.
Gastroscopy and colonoscopy in other hospital showed no abnormality.
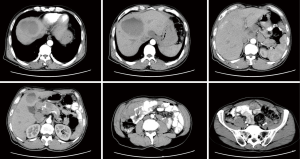
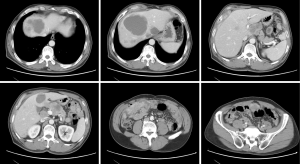
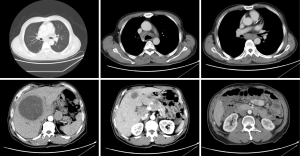
Abdominal and pelvic CT (on May 2, 2013, in our hospital): (I) a mass in neck of pancreas, which was considered as malignant; (II) multiple liver metastases; (III) multiple abdominal/pelvic cavity and retroperitoneal lymph node metastases; and (IV) omental metastasis (Figure 1).
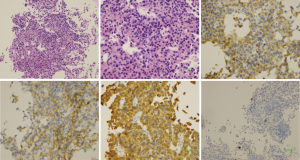
Ultrasound-guided puncture of the abdominal wall mass (on May 2, 2013): cytology showed the presence of tumor cells, and a diagnosis of a neuroendocrine tumor was considered based in combination with the immunochemical results.
Immunohistochemical findings: BerEp4(+++), calrentinin(+), Syn(++), CD56(±), and HME-1(−), CgA(±), MOC31(+++), and Ki-67(15%+).
Pathology: infiltration of an extremely small number of small round cell tumor cells was seen in fibrous tissue. In combination with clinical findings, the possibility of a metastasis with acinar differentiation was considered.
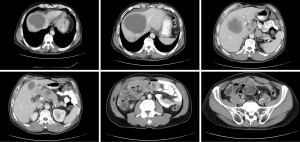
Immunohistochemical findings: AE1/AE3(3+), hepotocyte(−), CgA(2+), Syn(3+), Ki67(3%+), CD56(2+), NSE(3+), CD117(-), AAT(2+), and ACT(1+) (Figure 2).
Diagnosis: pancreatic neuroendocrine cancer with liver metastases and multiple peritoneal metastases.
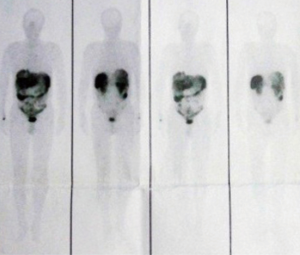
Somatostatin receptor scintigraphy (on May 7, 2013): high expression of somatostatin receptor was seen in pancreas, liver, and abdominal and pelvic cavities, which met the diagnostic criteria of neuroendocrine neoplasms (NENs) (Figure 3).
Multidisciplinary treatment (MDT) consultation on May 14, 2013 suggested that the diagnoses were pancreatic NEN (G2) with accompanying multiple abdominal and pelvic metastases and multiple hepatic metastases. Currently the disease was in a relatively advanced stage, and the patient also had the symptoms of carcinoid syndrome. A combined therapy with sandostatin and sutent was recommended. The patient then received routine follow-up examinations. He felt that his general conditions were better than before and the abdominal mass became smaller; the appetite increased and there was no diarrhea; bowel movement once a day, weight gain 10 pounds. He defecated once daily and his body weight increased by 5 kg.
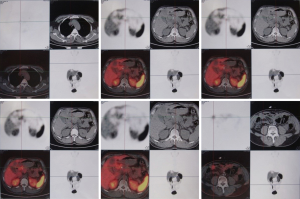
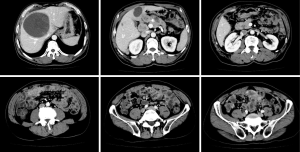
PET-CT after treatment is Figure 4 and comparison of abdominal CT findings before and after treatment is shown in Figures 5-8.
Sutent was withdrawn in July 2015 due to drug resistance. Currently the patient is not on any treatment.
Discussion
Pancreatic neuroendocrine tumor (pNET), formerly known as islet cell tumors, account for about 3% of primary pancreatic cancer. According to the hormone secretion status and the patient’s clinical presentations, pNET can be classified as functioning and non-functioning grading and prognosis (Tables 1,2).
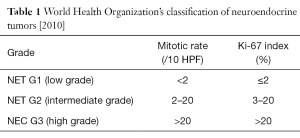
Full table
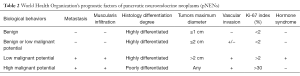
Full table
The common serological markers of pNET include chromogranin A (CgA) and neuron-specific enolase (NSE), whose abnormal increase often indicates the possibility of a neuroendocrine tumor. Medical imaging modalities such as contrast-enhanced CT and MRI are highly valuable for the diagnosis of pNET, which are mostly shown as hypervascular lesions with enhancement appearances at early arterial phase.
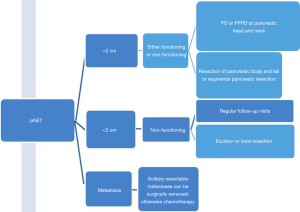
Multidisciplinary treatment of pNET (Figure 9)
Surgery
Liver metastasis accounts for about 90% of the distant metastases of pNET and is a major prognostic factor for this tumor. Research has shown that the concurrent resection of both the primary lesion and resectable liver metastases is feasible and can improve the prognosis (1). Palliative surgery refers to the removal of most of the metastasis (>90% of the lesion), during which the concurrent or staged resection of the primary lesion or liver metastases may be considered. If staged resection is performed, the liver metastases should be resected first, followed by the resection of the primary lesions, with an attempt to avoid the transfer of liver abscess and liver cancer cells from the biliary-enteric anastomosis to the intestinal tract (2). While liver transplantation is not a routine treatment for pNET, surgical methods can control symptoms and improve the prognosis.
Non-surgical treatment
Non-surgical approaches can be applied for advanced pNET with liver metastasis or multiple metastases. These approaches include medical treatment (e.g., biotherapy, molecularly targeted therapy, and chemotherapy), radiotherapy, and local treatments including radiofrequency ablation and arterial chemoembolization. These approaches can control symptoms, improve quality of life, and prolong survival. Among the medical treatments, biotherapy is mainly based on somatostatins. While somatostatin-based biotherapy has an objective response rate of <10% for pNET, the disease control rates range 50–60%. They are particularly useful for advanced pNET. Somatostatins (e.g., slow-release formulation of lanreotide and long-acting octreotide) can act on the somatostatin receptor on pNET cells and thus effectively alleviate and control the neuro-endocrine symptoms, inhibit the growth of pNET, and prolong survival (3). As shown in many retrospective studies and randomized prospective studies, somatostatins can be used in patients with slowly progressing pNETs (G1/G2) and somatostatin receptor-positive pancreatic neuroendocrine cancer (pNEC) (G3), with relatively mild adverse reactions. Among the medical treatments, the main molecularly targeted drugs include sunitinib and everolimus. The mammalian target of rapamycin (mTOR) signaling pathway gene is the common mutation in pNET, accounting for about 16%. Blocking this signaling pathway can inhibit the growth of parts of pNET. Everolimus is an orally administered mTOR inhibitor, whereas sunitinib is a multitargeted tyrosine kinase inhibitor and can prolong the disease-free progression of pNET (4). Both drugs have good efficacy and tolerance for advanced and metastatic pNET. Among the medical treatments, chemotherapy is not useful for neuroendocrine tumors. It can only be applied in patients with advanced tumors that are unresectable. The role of streptozotocin combined with 5-fluorouracil (5-FU) and/or epirubicin in treating G1/G2 pNENs has been well demonstrated and thus has become standard treatments. Temozolomide alone or in combination with capecitabine also has certain role in treating metastatic pancreatic neuroendocrine neoplasms (pNENs). Oxaliplatin or irinotecan can also be used as the second-line treatment options for pNENs. Radiotherapy is mainly used for brain or bone metastases. Among the local treatments, radiofrequency ablation and arterial interventional therapy have important roles in treating pNET with liver metastasis; they can effectively control the liver metastases and alleviate the neuroendocrine symptoms.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Cusati D, Zhang L, Harmsen WS, et al. Metastatic nonfunctioning pancreatic neuroendocrine carcinoma to liver: surgical treatment and outcomes. J Am Coll Surg 2012;215:117-24; discussion 124-5. [Crossref] [PubMed]
- De Jong MC, Farnell MB, Sclabas G, et al. Liver-directed therapy for hepatic metastases in patients undergoing pancreaticoduodenectomy: a dual-center analysis. Ann Surg 2010;252:142-8. [Crossref] [PubMed]
- Martín-Richard M, Massutí B, Pineda E, et al. Antiproliferative effects of lanreotide autogel in patients with progressive, well-differentiated neuroendocrine tumours: a Spanish, multicentre, open-label, single arm phase II study. BMC Cancer 2013;13:427. [Crossref] [PubMed]
- Raymond E, Dahan L, Raoul JL, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med 2011;364:501-13. [Crossref] [PubMed]
Cite this article as: Wang Y, Zhao D. Pancreatic neuroendocrine cancer with liver metastases and multiple peritoneal metastases: report of one case. Transl Gastroenterol Hepatol 2016;1:65.