Technical notes on pure laparoscopic isolated caudate lobectomy for patient with liver cancer
Introduction
The role of laparoscopic liver resection has been gaining more popularity and supports (1-3). It has been shown that with the same stage of disease, laparoscopic liver resection provides the same oncological clearance and survival benefit over open hepatectomy. In most of the literatures, laparoscopic liver resection demonstrated a shorter hospital stay, smaller incisions of wound, shorter operation times and most importantly less blood loss. Patients with hepatocellular carcinoma (HCC) and liver cirrhosis are no longer contraindication for pure laparoscopic liver resection (1,4-6). The number of major hepatectomy performed for liver cancer has also been increasing. Comparing to minor liver resection, the expertise requirement is much higher in major liver resection and thus the second international consensus meeting of laparoscopic liver resection stated that major hepatectomy can be performed by expert centers but more evidence is needed to support its role as a standard treatment for liver cancer (7). Surgeons who had experience in open hepatectomy for complicated cases have to acquire a new set of skills in order to perform safe surgery in laparoscopic approach.
A difficulty score of laparoscopic hepatectomy is thus needed which will guide the surgeons to performed laparoscopic liver resection according to their laparoscopic experience (8). Laparoscopic caudate lobectomy has been considered as one of the most difficult procedures in laparoscopic liver resection.
Surgical technique
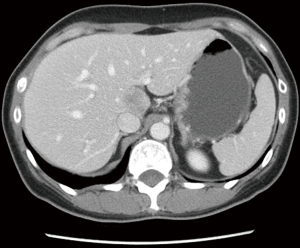
The patient was a 54-year-old lady who had carcinoma of the rectum with laparoscopic anterior resection performed. Adjuvant chemotherapy was given to her for 6 cycles. She was regularly followed up in the hospital with contrast CT scan of the abdomen performed every 6 months (Figure 1). A 2 cm lesion was found in the left caudate lobe of the liver 1 year after the colectomy. PET only revealed the caudate lobe lesion. There was no extrahepatic metastasis. The haemoglobin level was 11 g/dL and her platelet count was only 120×109/L.
Pure laparoscopic resection of the caudate lobe was proposed.
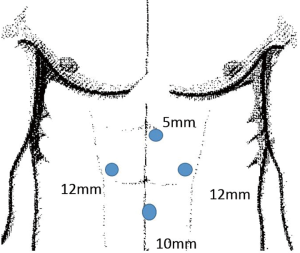
The patient was put on supine position with both leg spread opened (French position). The surgeon was standing in between the legs and one assistant was standing on patient’s left side. The 30 degree laparoscope was placed in subumbilical region. Two 12 mm ports and one 5 mm ports was introduced as working ports. 10 cm space was allowed between each port to avoid instrument interference (Figure 2). Pneumoperitoneum was created at 12 mmHg. Intraoperative ultrasound was performed to localized the lesion, confirmed the extension of the tumour and excluded the presence of additional nodule. The lesion was found only in the caudate lobe with close proximity to the inferior vena cava (IVC). The left lateral section of the liver was lift up by retractor through a 5 mm port. The peritoneal reflection was opened and the IVC was exposed (Figure 3A). A replaced left hepatic artery was identified during mobilization of the liver. The Spiegel’s lobe of caudate was mobilized and separated from the IVC by CUSA (Figure 3B). The short hepatic vessel was controlled with metal clips. Liver parenchymal transection was performed using the CUSA. The caudate pedicle was controlled by clips (Figure 3C). The IVC was fully exposed after the transection of the caudate lobe (Figure 3D). Bleeding from parenchymal transection was controlled with clips and diathermy. Bleeding from a branch of short hepatic and IVC was encountered. The bleeding site was controlled by grasping forceps and intracorporal suture was performed. The caudate lobectomy was completed by using the CUSA running anterior to the IVC surface. The specimen was put into a bag and delivered via enlargement of the subumbilical wound.
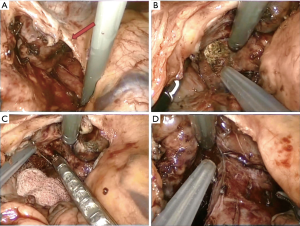
Pringle maneuver was not required and no drain was place after completion of caudate lobectomy. The procedure was recorded in multimedia format (Figure 4).

Results
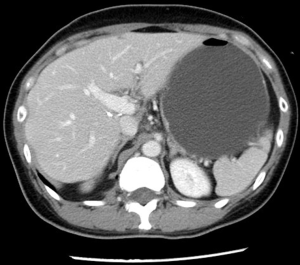
The operation last for 180 minutes. Blood loss was 220 mL and no blood transfusion was required. She resumed diet on the next day and was discharged 3 days after the operation. Histopathological examination showed 2 cm colorectal liver metastasis with a clear margin. Contrast CT scan performed 1 year after the operation showed no recurrence of the disease (Figure 5).
Discussion
Isolated caudate lobectomy has been considered as one of the most technically demanding surgery for liver surgeons even in open approaches. The caudate lobe lied posterior to the confluence of the left and middle hepatic veins as they entered the IVC. Any injury to these vital vessels will lead to massive bleeding (10,11).
Different approaches to isolated caudate lobectomy were reported. They were the posterior approach with or without total hepatic vascular exclusion described by Yanaga et al. (12); the left lateral approach described by Colonna et al. (13) and the anterior approach described by Yamamoto et al. (14) and modified anterior approach described by Cheung et al. (15).
The technical demand for caudate lobectomy in pure laparoscopic approach will be high as the anatomy of caudate lobe remains deep seated in the liver. The most reasonable way to resect the caudate lobe through pure laparoscopy is by left lateral approach. Big tumour mainly located in the right caudate process will not be a suitable candidate for left lateral approach. A right posterior approach or in association with formal right hepatectomy is required.
In pure laparoscopic approach, the surgeon has the benefit of looking at the caudate lobe from below. With today’s high definition display unit and with future 4k display unit, the anatomic structure including the small vessel branches can be visualized clearly with magnifications. The left lateral approach with a viewing angle from inferior end allowed minimal mobilization of the left lobe of the liver. The use of CUSA and modern energy devices which incorporated haemostasis and sealing ability enable effective and safer parenchymal transection.
The blood loss in this operation was only 220 mL. As a general principle in hepatectomy, the central venous pressure should be kept at below 5 cm water. The presence of pneumoperitoneum at 12 mmHg gave a very favorable negative gradient to prevent venous oozing during parenchymal transection. Pringle maneuver was not required during the operation. Little bleeding would be encountered as long as the parenchymal transection was at the anatomical boundaries of the caudate lobe.
The patient had a very small wound and most important of all, the lobectomy reviewed a clear margin. Minimal adhesion will be expected even if the patient required another surgery in future (16).
Conclusions
Pure laparoscopic lobectomy through a left lateral approach can be a safe treatment option for patients with caudate lobe tumour by surgeons with experience in laparoscopic surgery and complicated liver surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The video of this paper has been presented in the Morioka 2nd International Consensus Conference on Laparoscopic Liver Resection and won the best video award.
Ethical Statement: The study was approved by institutional ethic board and written informed consent was obtained from all patients.
References
- Han HS, Shehta A, Ahn S, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma: Case-matched study with propensity score matching. J Hepatol 2015;63:643-50. [Crossref] [PubMed]
- Cheung TT, Poon RT, Yuen WK, et al. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 2013;257:506-11. [Crossref] [PubMed]
- Wakabayashi G. Laparoscopic liver resection: how far can we go? J Hepatobiliary Pancreat Surg 2009;16:403-4. [Crossref] [PubMed]
- Cheung TT, Poon RT, Lo CM. Reply to Letter: "Long-term Survival Analysis of Pure Laparoscopic Versus Open Hepatectomy for Hepatocellular Carcinoma in Patients With Cirrhosis: A Single-center Experience Ann Surg 2015;262:e20-1. [Crossref] [PubMed]
- Cheung TT, Poon RT, Yuen WK, et al. Outcome of laparoscopic versus open hepatectomy for colorectal liver metastases. ANZ J Surg 2013;83:847-52. [Crossref] [PubMed]
- Kim KH, Jung DH, Park KM, et al. Comparison of open and laparoscopic live donor left lateral sectionectomy. Br J Surg 2011;98:1302-8. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Ban D, Tanabe M, Ito H, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 2014;21:745-53. [Crossref] [PubMed]
- Cheung TT. Pure laparoscopic resection of caudate lobe liver metastasis. Asvide 2016;3:255. Available online: http://www.asvide.com/articles/1015
- Liu P, Qiu BA, Bai G, et al. Choice of approach for hepatectomy for hepatocellular carcinoma located in the caudate lobe: isolated or combined lobectomy? World J Gastroenterol 2012;18:3904-9. [Crossref] [PubMed]
- Kosuge T, Yamamoto J, Takayama T, et al. An isolated, complete resection of the caudate lobe, including the paracaval portion, for hepatocellular carcinoma. Arch Surg 1994;129:280-4. [Crossref] [PubMed]
- Yanaga K, Matsumata T, Hayashi H, et al. Isolated hepatic caudate lobectomy. Surgery 1994;115:757-61. [PubMed]
- Colonna JO 2nd, Shaked A, Gelabert HA, et al. Resection of the caudate lobe through "bloody gultch". Surg Gynecol Obstet 1993;176:401-2. [PubMed]
- Yamamoto J, Kosuge T, Shimada K, et al. Anterior transhepatic approach for isolated resection of the caudate lobe of the liver. World J Surg 1999;23:97-101. [Crossref] [PubMed]
- Cheung TT, Yuen WK, Poon RT, et al. Improved anterior hepatic transection for isolated hepatocellular carcinoma in the caudate. Hepatobiliary Pancreat Dis Int 2014;13:219-22. [Crossref] [PubMed]
- Cheung TT, Ng KK, Poon RT, et al. A case of laparoscopic hepatectomy for recurrent hepatocellular carcinoma. World J Gastroenterol 2010;16:526-30. [Crossref] [PubMed]
Cite this article as: Cheung TT. Technical notes on pure laparoscopic isolated caudate lobectomy for patient with liver cancer. Transl Gastroenterol Hepatol 2016;1:56.