Successful en bloc resection of an esophageal hemangioma by combined EBL & EMR: a case report and technical review
Introduction
Esophageal hemangiomas are uncommon benign vascular tumor (1). Esophagectomy is the conventional surgical approach to treatment, but recently less invasive approaches by endoscopic mucosal resection (EMR) have become more widely used (2,3). EMR of esophageal hemangioma is rare. Endoscopic band ligation (EBL) have been used to management of variceal bleeding, but also been used to remove subepithelial tumor. There has been no report to treat esophageal hemangioma by EBL. EBL have less bleeding risk than other technique, and have more safety than EMR and endoscopic submucosal dissection (ESD).
In this case, we report here the first case of a submucosal esophageal hemangioma successfully removed en bloc by EBL and EMR.
Case representation
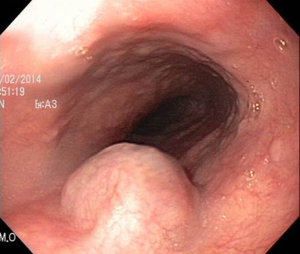
A 58-year-old male had no specific symptom. Upper gastroesophageal endoscopy in a periodic medical examination of other hospital revealed a 17 mm diameter subepithelial tumor 28 cm from incisor (Figure 1). The tumor size was increased than the past examination. The patient was referred to the department of gastroenterology in our hospital.
The patient’s physical and overall nutritive condition was good. There was no abnormal physical finding in the thoracic or abdominal regions. Edema of the lower extremities was not observed.
Concerning blood biochemistry, there were no abnormalities in peripheral blood, blood biochemistry, blood coagulation test findings, tumor markers, and viral markers.
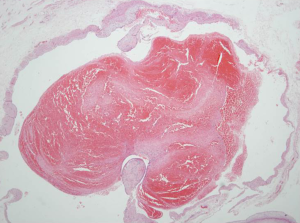
Endoscopic ultrasonography (EUS) revealed tumor with heterogeneous echogenicity and regular margin (Figure 2).
Contrast-enhanced computed tomography (CT) of the thoracic region revealed well-defined luminal protruding nodule at the mid-esophagus.
Combined EBL & EMR was performed for diagnostic treatment on July 24, 2014 (Figure 3). After EBL & EMR, there was no complication.
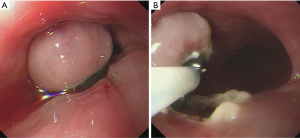
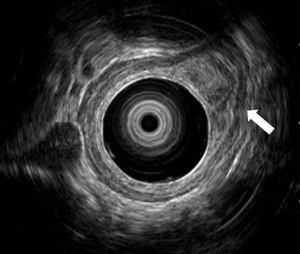
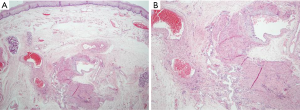
The resected specimen measuring 17 mm × 12 mm × 10 mm which consists of a piece of grayish white soft tissue. Histopathological results revealed hemangioma with organized hematoma (Figures 4,5). CD34 immunohistochemical staining was positive. Follow-up endoscopy was performed at 5 months later. There was no evidence of active bleeding at EMR site. The patient has now remained free of recurrence or complication for 5 months.
Discussion
Hemangioma is well known to arise from organs such as the skin, liver, kidney, and brain (4). Esophageal hemangiomas are rare benign vascular tumors (1) which represent around 3% of all benign esophageal tumors (5).
On CT, esophageal cavernous hemangiomas appear homogenous and isodense mass with calcification (6). EUS can be used to further determine the anatomy of the tumor. On EUS, hemangioma range from anechoic to hypoechoic to isoechoic and involve the mucosal and submucosal layers with intact muscularis propria (7).
Malignancy has been reported in some tumors predicating the surgical evaluation. But the risk of malignancy is greater with tumors more than 3 cm in size (8).
To treat esophageal hemangioma, esophagectomy or tumor enucleation has been performed. For surgery, thoracotomy should be performed, which is stressful for endoscopic treatment.
Endoscopic sclerotherapy is less stressful than surgery. It has been commonly applied to varices for both hemostasis of active bleeding and subsequent obliterative treatment (9). But endoscopic sclerotherapy may cause hemorrhage on puncture site and complication including the side effects of infused agents (3). Biopsy tissue is cannot be obtained by endoscopic sclerotherapy.
Another treatment is potassium titanyl/yttrium aluminium garnet (KTP/YAG) laser therapy. KTP/YAG laser was applied to a larger hemangioma as a less invasive strategy than surgery (10).
There was a case of a submucosal esophageal hemangioma successfully removed en bloc by ESD (1). ESD was performed under general anesthesia. An improved insulated-tip (IT-2) knife and a needle knife (dual knife) were used in this case. But ESD is too invasive to performed. ESD is too invasive treatment to perform because of serious complication such as perforation or bleeding.
Less invasive approaches by endoscopic therapy have become more widely used recently (2,3). Because, conventional endoscopic therapy cannot obtain specimens for pathological examination and is associated with a risk residual or recurrent hemangioma (11).
EMR is possible treatment option. Endoscopic resection is less invasive than ESD, and may reduce the risk of serious complication. However, EMR also cause bleeding during procedure.
Combined treatment of EBL and EMR for esophageal hemangioma may decrease bleeding risk of EMR alone. Combined EBL and EMR is less invasive than ESD or surgery and have advantage in bleeding control. The success of EMR in reducing the occurrence of bleeding is improved by its combination with EBL and EMR.
The number of patients undergoing EMR or endoscopic polypectomy is increasing, especially when the tumor is pedunculated and small in size (12). A large tumor may predicate the need for surgical resection (6).
There was no report to combined EBL and EMR for esophageal hemangioma. Combined EBL and EMR is alternative treatment option for esophageal hemangioma.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Kobara H, Mori H, Masaki T. Successful en bloc resection of an esophageal hemangioma by endoscopic submucosal dissection. Endoscopy 2012;44 Suppl 2 UCTN:E134-5.
- Cantero D, Yoshida T, Ito T, et al. Esophageal hemangioma: endoscopic diagnosis and treatment. Endoscopy 1994;26:250-3. [Crossref] [PubMed]
- Sogabe M, Taniki T, Fukui Y, et al. A patient with esophageal hemangioma treated by endoscopic mucosal resection: a case report and review of the literature. J Med Invest 2006;53:177-82. [Crossref] [PubMed]
- Lee JC, Kim JW, Lee YJ, et al. Cervical esophageal hemangioma combined with thyroid cancer. Korean J Thorac Cardiovasc Surg 2011;44:311-3. [Crossref] [PubMed]
- Plachta A. Benign tumors of the esophagus. Review of literature and report of 99 cases. Am J Gastroenterol 1962;38:639-52. [PubMed]
- Rajoriya N, D'costa H, Gupta P, et al. An unusual cause of dyspepsia: oesophageal cavernous haemangioma. QJM 2010;103:791-3. [Crossref] [PubMed]
- Tominaga K, Arakawa T, Ando K, et al. Oesophageal cavernous haemangioma diagnosed histologically, not by endoscopic procedures. J Gastroenterol Hepatol 2000;15:215-9. [Crossref] [PubMed]
- Bandoh T, Isoyama T, Toyoshima H. Submucosal tumors of the stomach: a study of 100 operative cases. Surgery 1993;113:498-506. [PubMed]
- Nagata-Narumiya T, Nagai Y, Kashiwagi H, et al. Endoscopic sclerotherapy for esophageal hemangioma. Gastrointest Endosc 2000;52:285-7. [Crossref] [PubMed]
- Shigemitsu K, Naomoto Y, Yamatsuji T, et al. Esophageal hemangioma successfully treated by fulguration using potassium titanyl phosphate/yttrium aluminum garnet (KTP/YAG) laser: a case report. Dis Esophagus 2000;13:161-4. [Crossref] [PubMed]
- Urakami T, Kondo K, Kasugai T, et al. A case of recurrent esophageal cavernous hemangioma increasing rapidly after surgery. Jpn J Thorac Cardiovasc Surg 1998;46:1206-10. [Crossref] [PubMed]
- Rasalkar DD, Chiu PW, Teoh AY, et al. Oesophageal haemangioma: imaging characteristics of this rare condition. Hong Kong Med J 2010;16:230-1. [PubMed]
Cite this article as: Baek IH, Jeon JW, Shin HP, Cha JM, Joo KR, Lee JI, Won KY, Min KW. Successful en bloc resection of an esophageal hemangioma by combined EBL & EMR: a case report and technical review. Transl Gastroenterol Hepatol 2016;1:45.